709
11
Human Health: Impacts,
Adaptation, and Co-Benefits
Coordinating Lead Authors:
Kirk R. Smith (USA), Alistair Woodward (New Zealand)
Lead Authors:
Diarmid Campbell-Lendrum (WHO), Dave D. Chadee (Trinidad and Tobago), Yasushi Honda
(Japan), Qiyong Liu (China), Jane M. Olwoch (South Africa), Boris Revich (Russian Federation),
Rainer Sauerborn (Sweden)
Contributing Authors:
Clara Aranda (Mexico), Helen Berry (Australia), Colin Butler (Australia), Zoë Chafe (USA),
Lara Cushing (USA), Kristie L. Ebi (USA), Tord Kjellstrom (New Zealand), Sari Kovats (UK),
Graeme Lindsay (New Zealand), Erin Lipp (USA), Tony McMichael (Australia), Virginia Murray
(UK), Osman Sankoh (Sierra Leone), Marie O’Neill (USA), Seth B. Shonkoff (USA),
Joan Sutherland (Trinidad and Tobago), Shelby Yamamoto (Germany)
Review Editors:
Ulisses Confalonieri (Brazil), Andrew Haines (UK)
Volunteer Chapter Scientists:
Zoë Chafe (USA), Joacim Rocklov (Sweden)
This chapter should be cited as:
Smith
, K.R., A. Woodward, D. Campbell-Lendrum, D.D. Chadee, Y. Honda, Q. Liu, J.M. Olwoch, B. Revich, and
R. Sauerborn, 2014: Human health: impacts, adaptation, and co-benefits. In: Climate Change 2014: Impacts,
Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the
Fifth Assessment Report of the Intergovernmental Panel on Climate Change [Field, C.B., V.R. Barros,
D.J. Dokken, K.J. Mach, M.D. Mastrandrea, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada, R.C. Genova,
B. Girma, E.S. Kissel, A.N. Levy, S. MacCracken, P.R. Mastrandrea, and L.L. White (eds.)]. Cambridge University
Press, Cambridge, United Kingdom and New York, NY, USA, pp. 709-754.

11
710
Executive Summary ........................................................................................................................................................... 713
11.1. Introduction ............................................................................................................................................................ 715
11.1.1. Present State of Global Health ......................................................................................................................................................... 715
11.1.2. Developments Since AR4 .................................................................................................................................................................. 715
Box 11-1. Weather, Climate, and Health: A Long-Term Observational Study in African and Asian Populations .......................... 715
11.1.3. Non-Climate Health Effects of Climate-Altering Pollutants ............................................................................................................... 716
11.2. How Climate Change Affects Health ....................................................................................................................... 716
11.3. Vulnerability to Disease and Injury Due to Climate Variability and Climate Change ............................................. 717
11.3.1. Geographic Causes of Vulnerability .................................................................................................................................................. 717
11.3.2. Current Health Status ....................................................................................................................................................................... 717
11.3.3. Age and Gender ............................................................................................................................................................................... 717
11.3.4. Socioeconomic Status ....................................................................................................................................................................... 718
11.3.5. Public Health and Other Infrastructure ............................................................................................................................................. 718
11.3.6. Projections for Vulnerability .............................................................................................................................................................. 718
11.4. Direct Impacts of Climate and Weather on Health ................................................................................................. 720
11.4.1. Heat- and Cold-Related Impacts ....................................................................................................................................................... 720
11.4.1.1. Mechanisms ...................................................................................................................................................................... 720
11.4.1.2. Near-Term Future .............................................................................................................................................................. 721
11.4.2. Floods and Storms ............................................................................................................................................................................ 721
11.4.2.1. Mechanisms ...................................................................................................................................................................... 722
11.4.2.2. Near-Term Future ............................................................................................................................................................... 722
11.4.3. Ultraviolet Radiation ......................................................................................................................................................................... 722
11.5. Ecosystem-Mediated Impacts of Climate Change on Health Outcomes ................................................................. 722
11.5.1. Vector-Borne and Other Infectious Diseases ..................................................................................................................................... 722
11.5.1.1. Malaria .............................................................................................................................................................................. 722
11.5.1.2. Dengue Fever .................................................................................................................................................................... 723
Box 11-2. Case Study: An Intervention to Control Dengue Fever .................................................................................... 724
11.5.1.3. Tick-Borne Diseases ........................................................................................................................................................... 725
11.5.1.4. Other Vector-Borne Diseases ............................................................................................................................................. 725
11.5.1.5. Near-Term Future ............................................................................................................................................................... 725
11.5.2. Food- and Water-Borne Infections .................................................................................................................................................... 726
11.5.2.1. Vibrios ............................................................................................................................................................................... 726
11.5.2.2. Other Parasites, Bacteria, and Viruses ................................................................................................................................ 726
11.5.2.3. Near-Term Future ............................................................................................................................................................... 727
Table of Contents

711
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
11.5.3. Air Quality ........................................................................................................................................................................................ 727
Box 11-3. Health and Economic Impacts of Climate-Altering Pollutants Other than CO
2
........................................................... 728
11.5.3.1. Long-Term Outdoor Ozone Exposures ............................................................................................................................... 728
11.5.3.2. Acute Air Pollution Episodes .............................................................................................................................................. 729
11.5.3.3. Aeroallergens .................................................................................................................................................................... 729
11.5.3.4. Near-Term Future ............................................................................................................................................................... 729
11.6. Health Impacts Heavily Mediated through Human Institutions ............................................................................. 730
11.6.1. Nutrition ........................................................................................................................................................................................... 730
11.6.1.1. Mechanisms ...................................................................................................................................................................... 730
11.6.1.2. Near-Term Future ............................................................................................................................................................... 730
11.6.2. Occupational Health ......................................................................................................................................................................... 731
11.6.2.1. Heat Strain and Heat Stroke .............................................................................................................................................. 731
11.6.2.2. Heat Exhaustion and Work Capacity Loss .......................................................................................................................... 731
11.6.2.3. Other Occupational Health Concerns ................................................................................................................................ 731
11.6.2.4. Near-Term Future ............................................................................................................................................................... 732
11.6.3. Mental Health ................................................................................................................................................................................... 732
11.6.4. Violence and Conflict ........................................................................................................................................................................ 732
11.7. Adaptation to Protect Health ................................................................................................................................. 733
11.7.1. Improving Basic Public Health and Health Care Services .................................................................................................................. 733
11.7.2. Health Adaptation Policies and Measures ......................................................................................................................................... 733
11.7.3. Early Warning Systems ...................................................................................................................................................................... 734
11.7.4. Role of Other Sectors in Health Adaptation ...................................................................................................................................... 734
11.8. Adaptation Limits Under High Levels of Warming .................................................................................................. 735
11.8.1. Physiological Limits to Human Heat Tolerance .................................................................................................................................. 736
11.8.2. Limits to Food Production and Human Nutrition .............................................................................................................................. 736
11.8.3. Thermal Tolerance of Disease Vectors ............................................................................................................................................... 736
11.8.4. Displacement and Migration Under Extreme Warming ..................................................................................................................... 736
11.8.5. Reliance on Infrastructure ................................................................................................................................................................. 736
11.9. Co-Benefits ............................................................................................................................................................. 737
11.9.1. Reduction of Co-Pollutants ............................................................................................................................................................... 737
11.9.1.1. Outdoor Sources ................................................................................................................................................................ 738
11.9.1.2. Household Sources ............................................................................................................................................................ 738
11.9.1.3. Primary Co-Pollutants ........................................................................................................................................................ 739
11.9.1.4. Secondary Co-Pollutants .................................................................................................................................................... 739
11.9.1.5. Case Studies of Co-Benefits of Air Pollution Reductions .................................................................................................... 740

712
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
11.9.2. Access to Reproductive Health Services ............................................................................................................................................ 740
11.9.2.1. Birth and Pregnancy Intervals ............................................................................................................................................ 740
11.9.2.2. Maternal Age at Birth ........................................................................................................................................................ 741
11.10. Key Uncertainties and Knowledge Gaps ................................................................................................................ 741
References ......................................................................................................................................................................... 743
Frequently Asked Questions
11.1: How does climate change affect human health? .............................................................................................................................. 741
11.2: Will climate change have benefits for health? .................................................................................................................................. 742
11.3: Who is most affected by climate change? ........................................................................................................................................ 742
11.4: What is the most important adaptation strategy to reduce the health impacts of climate change? ................................................. 742
11.5: What are health “co-benefits” of climate change mitigation measures? ......................................................................................... 742

713
11
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
Executive Summary
The health of human populations is sensitive to shifts in weather patterns and other aspects of climate change (very high
confidence). These effects occur directly, due to changes in temperature and precipitation and occurrence of heat waves, floods, droughts, and
fires. Indirectly, health may be damaged by ecological disruptions brought on by climate change (crop failures, shifting patterns of disease
vectors), or social responses to climate change (such as displacement of populations following prolonged drought). Variability in temperatures
is a risk factor in its own right, over and above the influence of average temperatures on heat-related deaths. {11.4} Biological and social
adaptation is more difficult in a highly variable climate than one that is more stable. {11.7}
Until mid-century climate change will act mainly by exacerbating health problems that already exist (very high confidence). New
conditions may emerge under climate change (low confidence), and existing diseases (e.g., food-borne infections) may extend their range into
areas that are presently unaffected (high confidence). But the largest risks will apply in populations that are currently most affected by climate-
related diseases. Thus, for example, it is expected that health losses due to climate change-induced undernutrition will occur mainly in areas
that are already food-insecure. {11.3}
In recent decades, climate change has contributed to levels of ill health (likely) though the present worldwide burden of ill health
from climate change is relatively small compared with other stressors on health and is not well quantified. Rising temperatures
have increased the risk of heat-related death and illness (likely). {11.4} Local changes in temperature and rainfall have altered distribution of
some water-borne illnesses and disease vectors, and reduced food production for some vulnerable populations (medium confidence). {11.5-6}
If climate change continues as projected across the Representative Concentration Pathway (RCP) scenarios, the major changes in ill health
compared to no climate change will occur through:
• Greater risk of injury, disease, and death due to more intense heat waves and fires (very high confidence) {11.4}
• Increased risk of undernutrition resulting from diminished food production in poor regions (high confidence) {11.6}
• Consequences for health of lost work capacity and reduced labor productivity in vulnerable populations (high confidence) {11.6}
• Increased risks of food- and water-borne diseases (very high confidence) and vector-borne diseases (medium confidence) {11.5}
• Modest reductions in cold-related mortality and morbidity in some areas due to fewer cold extremes (low confidence), geographical shifts
in food production, and reduced capacity of disease-carrying vectors due to exceedance of thermal thresholds (medium confidence). These
positive effects will be increasingly outweighed, worldwide, by the magnitude and severity of the negative effects of climate change (high
confidence). {11.4-6}
Impacts on health will be reduced, but not eliminated, in populations that benefit from rapid social and economic development
(high confidence), particularly among the poorest and least healthy groups (very high confidence). {11.4, 11.6-7}
Climate change is
an impediment to continued health improvements in many parts of the world. If economic growth does not benefit the poor, the health effects
of climate change will be exacerbated.
In addition to their implications for climate change, essentially all the important climate-altering pollutants (CAPs) other than
carbon dioxide (CO
2
) have near-term health implications (very high confidence). In 2010, more than 7% of the global burden of disease
was due to inhalation of these air pollutants (high confidence). {Box 11-4}
Some parts of the world already exceed the international standard for safe work activity during the hottest months of the year.
The capacity of the human body to thermoregulate may be exceeded on a regular basis, particularly during manual labor, in parts of the world
during this century. In the highest Representative Concentration Pathway, RCP8.5, by 2100 some of the world’s land area will be experiencing
4°C to 7°C higher temperatures due to anthropogenic climate change (WGI AR5 Figure SPM.7). If this occurs, the combination of high
temperatures and high humidity will compromise normal human activities, including growing food or working outdoors in some areas for
parts of the year (high confidence). {11.8}

714
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
The most effective measures to reduce vulnerability in the near term are programs that implement and improve basic public
health measures such as provision of clean water and sanitation, secure essential health care including vaccination and child
health services, increase capacity for disaster preparedness and response, and alleviate poverty (very high confidence). {11.7}
In addition, there has been progress since AR4 in targeted and climate-specific measures to protect health, including enhanced surveillance and
early warning systems. {11.7}
There are opportunities to achieve co-benefits from actions that reduce emissions of warming CAPs and at the same time improve health.
Among others, these include:
• Reducing local emissions of health-damaging and climate-altering air pollutants from energy systems, through improved energy efficiency,
and a shift to cleaner energy sources (very high confidence) {11.9}
• Providing access to reproductive health services (including modern family planning) to improve child and maternal health through birth
spacing and reduce population growth, energy use, and consequent CAP emissions over time (medium confidence) {11.9}
• Shifting consumption away from animal products, especially from ruminant sources, in high-meat-consumption societies toward less CAP-
intensive healthy diets (medium confidence) {11.9}
• Designing transport systems that promote active transport and reduce use of motorized vehicles, leading to lower emissions of CAPs and
better health through improved air quality and greater physical activity (high confidence). {11.9}
There are important research gaps regarding the health consequences of climate change and co-benefits actions, particularly in
low-income countries. There are now opportunities to use existing longitudinal data on population health to investigate how climate change
affects the most vulnerable populations. Another gap concerns the scientific evaluation of the health implications of adaptation measures at
community and national levels. A further challenge is to improve understanding of the extent to which taking health co-benefits into account
can offset the costs of greenhouse gas mitigation strategies.

715
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
11.1. Introduction
This chapter examines what is known about the effects of climate
change on human health and, briefly, the more direct impacts of climate-
a
ltering pollutants (CAPs; see Glossary) on health. We review diseases
and other aspects of poor health that are sensitive to weather and
climate. We examine the factors that influence the susceptibility of
populations and individuals to ill health due to variations in weather
and climate, and describe steps that may be taken to reduce the impacts
of climate change on human health. The chapter also includes a section
on health “co-benefits.” Co-benefits are positive effects on human
health that arise from interventions to reduce emissions of those CAPs
that warm the planet or vice versa.
This is a scientific assessment based on best available evidence according
to the judgment of the authors. We searched the English-language
literature up to August 2013, focusing primarily on publications since
2007. We drew primarily (but not exclusively) on peer-reviewed journals.
Literature was identified using a published protocol (Hosking and
Campbell-Lendrum, 2012) and other approaches, including extensive
consultation with technical experts in the field. We examined recent
substantial reviews (e.g., Gosling et al., 2009; Bassil and Cole, 2010;
Hajat et al., 2010; Huang et al., 2011; McMichael, 2013b; Stanke et al.,
2013) to check for any omissions of important work. In selecting citations
for the chapter, we gave priority to publications that were recent (since
AR4), comprehensive, added significant new findings to the literature,
and included areas or population groups that have not previously been
well described or were judged to be particularly policy relevant in other
respects.
We begin with an outline of measures of human health, the major driving
forces that act on health worldwide, recent trends in health status, and
health projections for the remainder of the 21st century.
11.1.1. Present State of Global Health
The Fourth Assessment Report (AR4) pointed to dramatic improvement
in life expectancy in most parts of the world in the 20th century, and
this trend has continued through the first decade of the 21st century
(Wang et al., 2012). Rapid progress in a few countries (especially China)
has dominated global averages, but most countries have benefited from
substantial reductions in mortality. There remain sizable and avoidable
inequalities in life expectancy within and between nations in terms of
education, income, and ethnicity (Beaglehole and Bonita, 2008) and in
some countries, official statistics are so patchy in quality and coverage
that it is difficult to draw firm conclusions about health trends (Byass,
2010). Years lived with disability have tended to increase in most
countries (Salomon et al., 2012).
If economic development continues as forecast, it is expected that
mortality rates will continue to fall in most countries; the World Health
Organization (WHO) estimates the global burden of disease (measured
in disability adjusted life years per capita) will decrease by 30% by 2030,
compared with 2004 (WHO, 2008a). The underlying causes of global
poor health are expected to change substantially, with much greater
prominence of chronic diseases and injury; nevertheless, the major
i
nfectious diseases of adults and children will remain important in some
regions, particularly sub-Saharan Africa and South Asia (Hughes et al.,
2011).
11.1.2. Developments Since AR4
The relevant literature has grown considerably since publication of AR4.
For instance, the annual number of MEDLINE citations on climate
change and health doubled between 2007 and 2009 (Hosking and
Campbell-Lendrum, 2012). In addition, there have been many reviews,
reports, and international assessments that do not appear in listings
such as MEDLINE but include important information nevertheless, for
instance, the World Development Report 2010 (World Bank, 2010) and
the 2011 UN Habitat report on cities and climate change (UN-HABITAT,
2011). Since AR4, there have been improvements in the methods applied
to investigate climate change and health. These include more sophisticated
modeling of possible future impacts (e.g., work linking climate change,
food security, and health outcomes; Nelson et al., 2010) and new methods
Box 11-1 | Weather, Climate, and Health:
A Long-Term Observational Study
in African and Asian Populations
Given the dearth of scientific evidence of the relationship
between weather/climate and health in low- and middle-
income countries, we report on a project that spans sub-
Saharan Africa and Asia. The INDEPTH Network currently
includes 43 surveillance sites in 20 countries. Using
standardized health and demographic surveillance systems,
member sites have collected up to 45 years of information
on births, migrations, and deaths. Currently, there are about
3.2 million people under surveillance (Sankoh and Byass,
2012).
To study relationships between weather and health, the
authors obtained daily meteorological data for 12 INDEPTH
populations between 2000 and 2009, and projected future
climate changes to 2100 under the SRES A1B, A3, and B1
scenarios (Hondula et al., 2012). The authors concluded the
health of all the populations would be challenged by the
new climatic conditions, especially later in the century. In
another study from the Network, Diboulo et al. (2012)
examined the relation between weather and all-cause
mortality data in Burkina Faso. Relations between daily
temperature and mortality were similar to those reported in
many high-income settings, and susceptibility to heat
varied by age and gender.
716
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
t
o model the effects of heat on work capacity and labor productivity
(Kjellstrom et al., 2009b). Other developments include coupling of high-
quality, longitudinal mortality data sets with down-scaled meteorological
data, in low-income settings (e.g., through the INDEPTH Network; see
Box 11-1).
Since AR4, studies of the ways in which policies to reduce greenhouse
gas (GHG) emissions may affect health, or vice versa, leading to so-
called “co-benefits” in the case of positive outcomes for either climate
or health, have multiplied (Haines et al., 2009).
Much has been written on links between climate, socioeconomic
conditions, and health—for example, related to occupational heat
exposure (Kjellstrom et al., 2009b) and malaria (e.g., Gething et al., 2010;
Béguin et al., 2011). There is also growing appreciation of the social
upheaval and damage to population health that may arise from the
interaction of large-scale food insecurity, population dislocation, and
conflict (see Chapter 12).
11.1.3. Non-Climate Health Effects
of Climate-Altering Pollutants
CAPs affect health in other ways than through climate change, just
as carbon dioxide (CO
2
) creates non-climate effects such as ocean
acidification. The effects of rising CO
2
levels on calcifying marine species
a
re well documented and the risks for coral reefs are now more closely
defined than they were at the time of the AR4 (see Chapter 30). There
are potential implications for human health, such as undernutrition in
coastal populations that depend on local fish stocks, but, so far, links
between health and ocean acidification have not been closely studied
(Kite-Powell et al., 2008). CAPs such as black carbon and tropospheric
ozone have substantial, direct, negative effects on human health (Wang
et al., 2013; see Section 11.5.3 and Box 11-3). Although CO
2
is not
considered a health-damaging air pollutant at levels experienced
outside particular occupational and health-care settings, one study has
reported a reduction in mental performance at 1000 ppm and above,
within the range that all of humanity would experience in some extreme
climate scenarios by 2100 (Satish et al., 2012).
11.2. How Climate Change Affects Health
There are three basic pathways by which climate change affects health
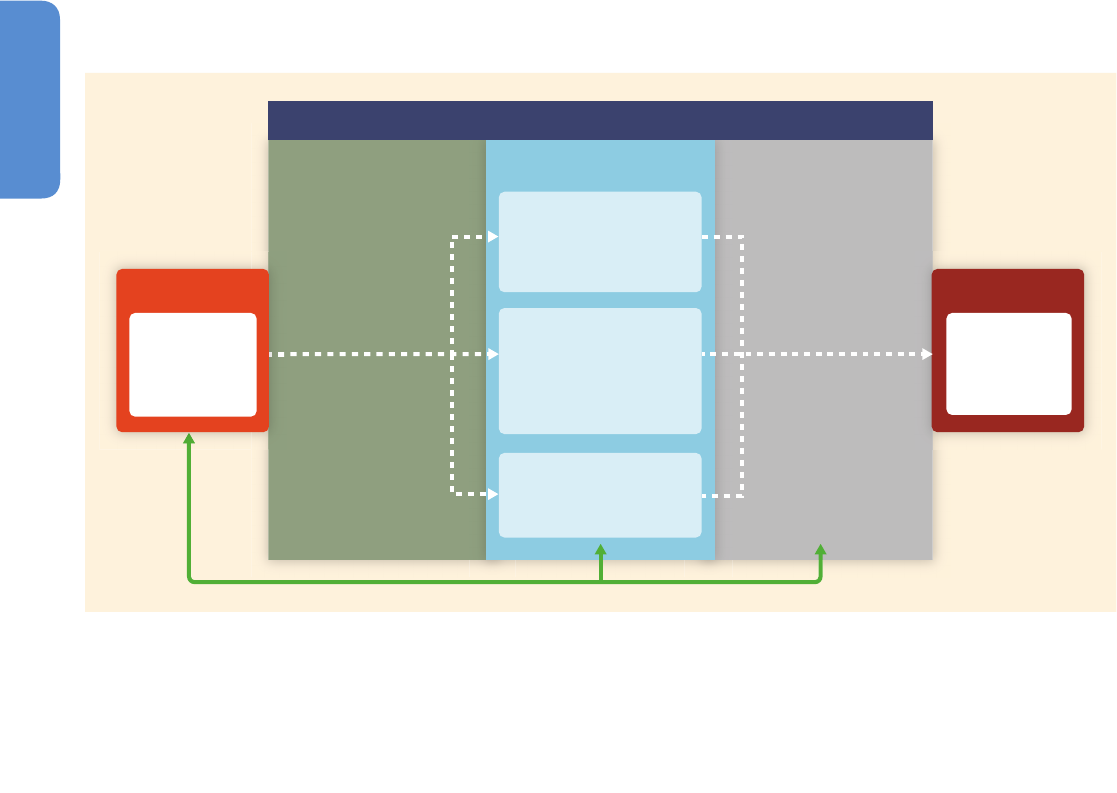
(Figure 11-1), and these provide the organization for the chapter:
• Direct impacts, which relate primarily to changes in the frequency
of extreme weather including heat, drought, and heavy rain (Section
11.4)
• Effects mediated through natural systems, for example, disease
vectors, water-borne diseases, and air pollution (Section 11.5)
• Effects heavily mediated by human systems, for example, occupational
impacts, undernutrition, and mental stress (Section 11.6).
• Warning systems
• Socioeconomic status
• Health and nutrition status
• Primary health care
• Geography
• Baseline weather
• Soil/dust
• Vegetation
• Baseline air/water
quality
Public health capability
and adaptation
Environmental
conditions
Social infrastructure
Direct exposures
Indirect exposures
Via economic and social disruption
• Food production/distribution
• Mental stress
Mediated through natural systems:
• Allergens
• Disease vectors
• Increased water/air pollution
• Flood damage
• Storm vulnerability
• Heat stress
HEALTH IMPACTS
• Undernutrition
• Drowning
• Heart disease
• Malaria
•
•
•
CLIMATE CHANGE
• Precipitation
• Heat
• Floods
• Storms
Mediating factors
Figure 11-1 |
Conceptual diagram showing three primary exposure pathways by which climate change affects health: directly through weather variables such as heat and
storms; indirectly through natural systems such as disease vectors; and pathways heavily mediated through human systems such as undernutrition. The green box indicates the
moderating influences of local environmental conditions on how climate change exposure pathways are manifest in a particular population. The gray box indicates that the extent
to which the three categories of exposure translate to actual health burden is moderated by such factors as background public health and socioeconomic conditions, and
adaptation measures. The green arrows at the bottom indicate that there may be feedback mechanisms, positive or negative, between societal infrastructure, public health, and
adaptation measures and climate change itself. As discussed later in the chapter, for example, some measures to improve health also reduce emissions of climate-altering
pollutants, thus reducing the extent and/or pace of climate change as well as improving local health (courtesy of E. Garcia, UC Berkeley). The examples are indicative.

717
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
T
he negative effects of climate change on health may be reduced by
improved health services, better disaster management, and poverty
alleviation, although the cost and effort may be considerable (Section
11.7). The consequences of large magnitude climate change beyond
2050, however, would be much more difficult to deal with (Section
11.8). Although there are exceptions, to a first approximation climate
change acts to exacerbate existing patterns of ill health, by acting on
the underlying vulnerabilities that lead to ill health even without climate
change. Thus, before pursuing the three pathways in Figure 11-1, we
summarize what is known about vulnerability to climate-induced illness
and injury.
11.3. Vulnerability to Disease and Injury Due to
Climate Variability and Climate Change
In the IPCC assessments, vulnerability is defined as the propensity or
predisposition to be adversely affected (see Chapter 19 and Glossary).
In this section, we consider causes of vulnerability to ill health
associated with climate change and climate variability, including
individual and population characteristics and factors in the physical
environment.
We have outlined the causes of vulnerability separately, but in practice
causes combine, often in a complex and place-specific manner. There are
some factors (such as education, income, health status, and responsiveness
of government) that act as generic causes of vulnerability. For example,
the quality of governance—how decisions are made and put into
practice—affects a community’s response to threats of all kinds (Bowen
et al., 2012; see Chapter 12). The background climate-related disease
rate of a population is often the best single indicator of vulnerability to
climate change—doubling of risk of disease in a low disease population
has much less absolute impact than doubling of the disease when the
background rate is high. (Note that here, and elsewhere in the chapter,
we treat “risk” in the epidemiological sense: the probability that an
event will occur.) But the precise causes of vulnerability, and therefore
the most relevant adaptation capacities, vary greatly from one setting
to another. For example, severe drought in Australia has been linked to
psychological distress—but only for those residing in rural and remote
areas (Berry et al., 2010). The link between high ambient temperatures
and increased incidence of salmonella food poisoning has been
demonstrated in many places (e.g., Zhang et al., 2010), but the lag
varies from one country to another, suggesting that the mechanisms
differ. Deficiencies in food storage may be the critical link in some
places; food handling problems may be most important elsewhere
(Kovats et al., 2004).
The 2010 World Development Report concluded that all developing
regions are vulnerable to economic and social damage resulting from
climate change—but for different reasons (World Bank, 2010). The
critical factors for sub-Saharan Africa, for example, are the current climate
stresses (in particular, droughts and floods) that may be amplified in
parts of the region under climate change, sparse infrastructure, and
high dependence on natural resources (see Chapter 22). Asia and the
Pacific, on the other hand, are distinguished by the very large number
of people living in low-lying areas prone to flooding (see Chapters 24
and 29).
11.3.1. Geographic Causes of Vulnerability
Location has an important influence on the potential for health losses
caused by climate change (Samson et al., 2011). Those working outdoors
in countries where temperatures in the hottest time of the year are
already at the limits of thermal tolerance for part of the year will be more
severely affected by further warming than workers in cooler countries
(Kjellstrom et al., 2013). The inhabitants of low-lying coral atolls are
very sensitive to flooding, contamination of freshwater reservoirs due
to sea level rise, and salination of soil, all of which may have important
effects on health (Nunn, 2009). Rural populations that rely on subsistence
farming in low rainfall areas are at high risk of undernutrition and
water-related diseases if drought occurs, although this vulnerability may
be modified strongly by local factors, such as access to markets and
irrigation facilities (Acosta-Michlik et al., 2008). Living in rural and
remote areas may confer increased risk of ill health because of limited
access to services and generally higher levels of social and economic
disadvantage (Smith, 2008). Populations that are close to the present
limits of transmission of vector-borne diseases are most vulnerable to
changes in the range of transmission as a result of rising temperatures
and altered patterns of rainfall, especially when disease control systems
are weak (Zhou et al., 2008; Lozano-Fuentes et al., 2012.). In cities, those
who live on urban heat islands are at greater risk of ill health due to
extreme heat events (Stone et al., 2010; Uejio et al., 2011).
11.3.2. Current Health Status
Climate extremes may promote the transmission of certain infectious
diseases, and the vulnerability of populations to these diseases will
depend on the baseline levels of pathogens and their vectors. In the USA,
as one example, arboviral diseases such as dengue are rarely seen after
flooding, compared with the experience in other parts of the Americas.
The explanation lies in the scarcity of dengue (and other pathogenic
viruses) circulating in the population, before the flooding (Keim, 2008). On
the other hand, the high prevalence of HIV infection in many populations
in sub-Saharan Africa will tend to multiply the health risks of climate
change, due to the interactions between chronic ill health, poverty,
extreme weather events, and undernutrition (Ramin and McMichael,
2009). Chronic diseases such as diabetes and ischemic heart disease
magnify the risk of death or severe illness associated with high ambient
temperatures (Basu and Ostro, 2008; Sokolnicki et al., 2009).
11.3.3. Age and Gender
Children, young people, and the elderly are at increased risk of climate-
related injury and illness (Perera, 2008). For example, adverse effects of
malaria, diarrhea, and undernutrition are presently concentrated among
children, for reasons of physiological susceptibility (Michon et al., 2007).
In principle, children are thought to be more vulnerable to heat-related
illnesses, owing to their small body mass to surface area ratio, but
evidence of excess heat-related mortality in this age group is mixed
(Basu and Ostro, 2008; Kovats and Hajat, 2008). Maternal antibodies
acquired in utero provide some protection against dengue fever in the
first year of life, but if infection does occur in infants it is more likely to
provoke the severe hemorrhagic form of illness (Ranjit and Kissoon,

718
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
2
011). Children are generally at greater risk when food supplies are
restricted: households with children tend to have lower than average
incomes, and food insecurity is associated with a range of adverse
health outcomes among young children (Cook and Frank, 2008).
Older people are at greater risk from storms, floods, heat waves, and
other extreme events (Brunkard et al., 2008), in part because they tend
to be less mobile than younger adults and so find it more difficult to
avoid hazardous situations and also because they are more likely to live
alone in some cultures. Older people are also more likely to suffer from
health conditions that limit the body’s ability to respond to stressors
such as heat and air pollution (Gamble et al., 2013).
The relationship between gender and vulnerability is complex. Worldwide,
mortality due to natural disasters, including droughts, floods, and storms,
is higher among women than men (WHO, 2011). However, there is
variation regionally. In the USA, males are at greater risk of death
following flooding (Jonkman and Kelman, 2005). A study of the health
effects of flooding in Hunan province, China, also found an excess of
flood deaths among males, often related to rural farming (Abuaku et
al., 2009). In Canada’s Inuit population males are exposed to dangers
associated with insecure sea ice, while females may be more vulnerable
to the effects of diminished food supplies (Pearce et al., 2011). In the
Paris 2003 heat wave, excess mortality was greater among females
overall, but there were more excess deaths among men in the working
age span (25 to 64) possibly due to differential exposures to heat in
occupational settings (Fouillet et al., 2006). In Bangladesh, females
are more affected than males by a range of climate hazards, due to
differences in prevalence of poverty, undernutrition, and exposure to
water-logged environments (Neelormi et al., 2009). The effect of food
insecurity on growth and development in childhood may be more
damaging for girls than boys (Cook and Frank, 2008).
Pregnancy is a period of increased vulnerability to a wide range of
environmental hazards, including extreme heat (Strand et al., 2012) and
infectious diseases such as malaria, foodborne infections, and influenza
(Van Kerkhove et al., 2011).
11.3.4. Socioeconomic Status
The poorest countries and regions are generally most susceptible to
damage caused by climate extremes and climate variability (Malik et
al., 2012), but wealthy countries are not immune, as shown by the
deaths resulting from bushfires in Australia in 2009 (Teague et al., 2010).
Also, rapid economic development may increase the risks of climate-
related health issues. For instance, changes in Tibet Autonomous Region,
China, including new roads and substantial in-migration may explain
(along with above-average warming) the appearance and establishment
in Lhasa of Culex pipiens, a mosquito capable of transmitting the West
Nile virus (Liu et al., 2013b).
A review of global trends in tropical cyclones 1970–2009 found that
mortality risk at country-level depended most strongly on three factors:
storm intensity, quality of governance, and levels of poverty (Peduzzi et
al., 2012). Individuals and households most vulnerable to climate hazards
tend to be those with relatively low socioeconomic status (Friel et al.,
2
008). A study of the impacts of flooding in Bangladesh found that
household risk reduced with increases in both average income and
number of income sources. Poorer households were not only more
severely affected by flooding, but they also took preventive action less
often and received assistance after flooding less frequently than did
more affluent households (Brouwer et al., 2007).
In many countries, race and ethnicity are powerful markers of health
status and social disadvantage. Black Americans have been reported to
be more vulnerable to heat-related deaths than other racial groups in
the USA (Basu and Ostro, 2008). This may be due to a higher prevalence
of chronic conditions such as overweight and diabetes (Lutsey et al.,
2010), financial circumstances (e.g., lower incomes may restrict access
to air conditioning during heat-waves; Ostro et al., 2010), or community-
level characteristics such as higher local crime rates or disrupted social
networks (Browning et al., 2006). Indigenous peoples who depend
heavily on local resources, and live in parts of the world where the
climate is changing quickly, are generally at greater risk of economic
losses and poor health. Studies of the Inuit people, for example, show
that rapid warming of the Canadian Arctic is jeopardizing hunting and
many other day-to-day activities, with implications for livelihoods and
well-being (Ford, 2009).
11.3.5. Public Health and Other Infrastructure
Populations that do not have access to good quality health care and
essential public health services are more likely to be adversely affected
by climate variability and climate change (Frumkin and McMichael,
2008). Harsh economic conditions in Europe since 2008 led to cutbacks
in health services in some countries, followed by a resurgence of
climate-sensitive infectious diseases including malaria (Karanikolos et
al., 2013). The condition of the physical infrastructure that supports
human settlements also influences health risks (this includes supply of
power, provision of water for drinking and washing, waste management,
and sanitation; see Chapter 8). In Cuba, a country with a well-developed
public health system, dengue fever has been a persistent problem in
the larger cities, due in part to the lack of a constant supply of drinking
water in many neighborhoods (leading to people storing water in
containers that are suitable breeding sites for the disease vector Aedes
aegypti; Bulto et al., 2006). In New York, daily mortality spiked after a
city-wide power failure in August 2003, due in part to increased exposure
to heat (Anderson and Bell, 2012).
11.3.6. Projections for Vulnerability
Population growth is linked to climate change vulnerability. If nothing
else changes, increasing numbers of people in locations that are already
resource poor and are affected by climate risks will magnify harmful
impacts. Virtually all the projected growth in populations will occur in
urban agglomerations, mostly in large, low latitude hot countries in
which a high proportion of the workforce is deployed outdoors with little
protection from heat. About 150 million people currently live in cities
affected by chronic water shortages and by 2050, unless there are rapid
improvements in urban environments, the number will rise to almost a
billion (McDonald et al., 2011). Under a “business as usual” scenario
719
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
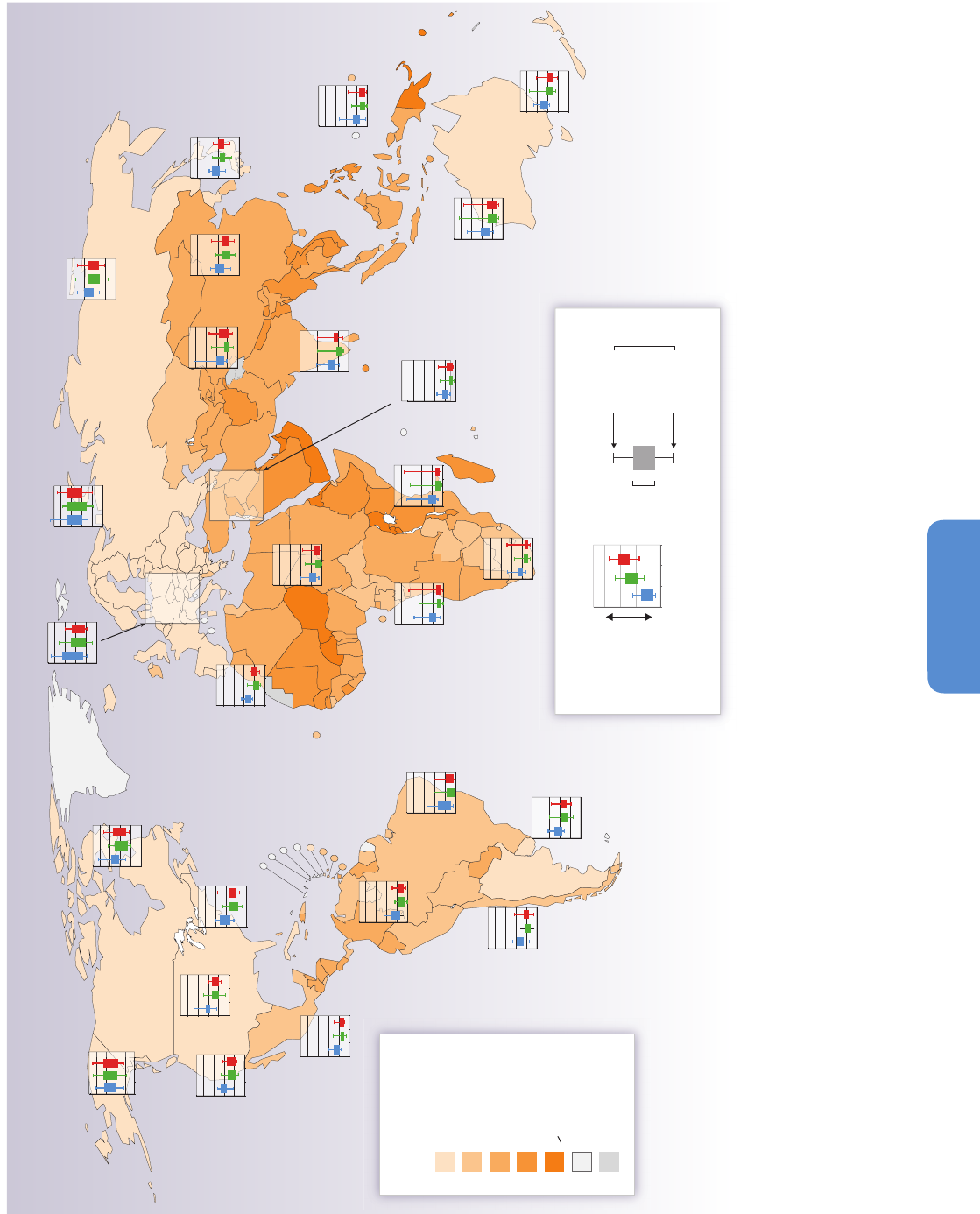
Population increase factor
(2010 to 2050)
1 to 2.99
3 to 4.99
5 to 6.99
7 to 9.99
>
10
Data not available
Not applicable
Higher frequency
Lower frequency
SRES Scenario
Maximum
projection
Minimum
projection
F
ull model range
50% of model
projections
Scenarios: B1 A1B A2
Mid-21st century projection
Figure 11-2 |
Increasingly frequent heat extremes will combine with rapidly growing numbers of older people living in cities—who are particularly vulnerable to extreme heat. Countries are shaded according to the expected proportional
increase in urban populations aged over 65 by the year 2050. Bar graphs show how frequently the maximum daily temperature that would have occurred only once in 20 years in the late 20th century is expected to occur in the mid-21st
century, with lower numbers indicating more frequent events. Results are shown for three different Special Report on Emission Scenarios (SRES) scenarios (blue = B1; green = A1B, red = A2), as described in the IPCC Special Report on
Emissions Scenarios, and based on 12 global climate models participating in the third phase of the Coupled Model Intercomparison Project (CMIP3). Colored boxes show the range in which 50% of the model projections are contained, and
whiskers show the maximum and minimum projections from all models (WHO and WMO, 2012).
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
1
4
16
Alaska/Northwest Canada
East Canada/Greenland/Iceland
East North America
Central North America
West North America
Central America/Mexico
Amazon
Northeast Brazil
West Coast South America
Southeast South America
South Africa
West Africa
East Africa
Sahara
South Europe/
Mediterranean
North Europe
North Asia
Central Asia Tibetan Plateau East Asia
South Asia
North Australia
South Australia/New Zealand
West Asia
Central Europe
Southeast Asia

720
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
w
ith mid-range population growth, the Organisation for Economic
Co-operation and Development (OECD) projects that about 1.4 billion
people will be without access to basic sanitation in 2050 (OECD, 2012).
The age structure of the population also has implications for vulnerability
(see Figure 11-2). The proportion aged over 60, worldwide, is projected
to increase from about 10% presently to about 32% by the end of the
century (Lutz et al., 2008). The prevalence of overweight and obesity,
which is associated with relatively poor heat tolerance, has increased
almost everywhere in the last 20 years, and in many countries the trend
continues upwards (Finucane et al., 2011). It has been pointed out that
the Sahel region of Africa may be particularly vulnerable to climate change
because it already suffers so much stress from population pressure,
chronic drought, and governmental instability (Diffenbaugh and Giorgi,
2012; Potts and Henderson, 2012).
Future trends in social and economic development are critically important
to vulnerability. For instance, countries with a higher Human Development
Index (HDI)—a composite of life expectancy, education, literacy, and gross
domestic product (GDP) per capita—are less affected by the floods,
droughts, and cyclones that take place (Patt et al., 2010). Therefore policies
that boost health, education, and economic development should reduce
future vulnerability. Overall, there have been substantial improvements
in HDI in the last 30 years, but this has been accompanied by increasing
inequalities between and within countries, and has come at the cost of
high consumption of environmental resources (UNDP, 2011).
11.4. Direct Impacts of Climate
and Weather on Health
11.4.1. Heat- and Cold-Related Impacts
Although there is ample evidence of the effects of weather and climate
on health, there are few studies of the impacts of climate change itself.
(An example: Bennett et al. (2013) reported that the ratio of summer
to winter deaths in Australia increased between 1968 and 2010, in
association with rising annual average temperatures.) The issue is scale,
as climate change is defined in decades. Robust studies require not only
extremely long-term data series on climate and disease rates, but also
information on other established or potential causative factors, coupled
with statistical analysis to apportion changes in health states to the
various contributing factors. Wherever risks are identified, health agencies
are mandated to intervene immediately, biasing long-term analyses.
Nevertheless, the connection between weather and health impacts is
often sufficiently direct to permit strong inferences about cause and
effect (Sauerborn and Ebi, 2012). Most notably, the association between
hot days (commonly defined in terms of the percentiles of daily maximum
temperature for a specified location) and increases in mortality is very
robust (Honda et al., 2013). The IPCC Special Report on Extreme Events
(SREX) concludes that it is very likely that there has been an overall
decrease in the number of cold days and nights, and an overall increase
in the number of warm days and nights, at the global scale. If there has
been an increase in daily maximum temperatures, then it follows, in our
view, that the number of heat-related deaths is likely to have also
increased. For example, Christidis et al. (2012) concluded that it is
“extremely likely (probability greater than 95%)” that anthropogenic
c
limate change at least quadrupled the risk of extreme summer heat
events in Europe in the decade 1999–2008. The 2003 heat wave was
one such record event; therefore, the probability that particular heat
wave can be attributed to climate change is 75% or more, and on this
basis it is likely the excess mortality attributed to the heat wave (about
15,000 deaths in France alone (Fouillet et al., 2008)) was caused by
anthropogenic climate change.
The rise in minimum temperatures may have contributed to a decline
in deaths associated with cold spells; however, the influence of seasonal
factors other than temperature on winter mortality suggests that the
impacts on health of more frequent heat extremes greatly outweigh
benefits of fewer cold days (Kinney et al., 2012; Ebi and Mills, 2013).
Quantification, globally, remains highly uncertain, as there are few studies
of the large developing country populations in the tropics, and these
point to effects of heat, but not cold, on mortality (Hajat et al., 2010).
There is also significant uncertainty over the degree of physiological,
social, or technological adaptation to increasing heat over long time
periods.
11.4.1.1. Mechanisms
The basic processes of human thermoregulation are well understood.
If the body temperature rises above 38°C (“heat exhaustion”), physical
and cognitive functions are impaired; above 40.6°C (“heat stroke”),
risks of organ damage, loss of consciousness, and death increase
sharply. Detailed exposure-response relationships were described long
ago (Wyndham, 1969), but the relationships in different community
settings and for different age/sex groups are not yet well established.
The early studies are supported by more recent experimental and field
studies (Ramsey and Bernard, 2000; Parsons, 2003) and meta-analysis
(Bouchama et al., 2007) that show significant effects of heat stress as
body temperatures exceed 40°C, and heightened vulnerability in
individuals with preexisting disease.
At high temperatures, displacement of blood to the surface of the body
may lead to circulatory collapse. Indoor thermal conditions, including
ventilation, humidity, radiation from walls or ceiling, and the presence
or absence of air conditioning, are important in determining whether
adverse events occur, but these variables are seldom well-measured in
epidemiological studies (Anderson et al., 2012). Biological mechanisms
are less evident for other causes of death, such as suicide, that are
sometimes related to high temperature (Page et al., 2007; Kim et al.,
2011; Likhvar et al., 2011).
Heat waves refer to a run of hot days; precisely how many days, and
how high the temperatures must rise, are defined variously (Kinney et
al., 2008). Some investigators have reported that mortality increases
more during heat waves than would be anticipated solely on the basis
of the short-term temperature mortality relationship (D’Ippoliti et al.,
2010; Anderson and Bell, 2011), although the added effect is relatively
small in some series, and most evident with prolonged heat waves
(Gasparrini and Armstrong, 2011). Because heat waves are relatively
infrequent compared with the total number of days with temperatures
greater than the optimum for that location, the effects of heat waves
are only a fraction of the total impact of heat on health. Some studies

721
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
h
ave shown larger effects of heat and heat waves earlier in the hot
season (Anderson and Bell, 2011; Rocklov et al., 2011). This may be
testament to the importance of acclimatization and adaptive measures,
or may result from a large group in the population that is more susceptible
to heat early in the season (Rocklov et al., 2009, 2011).
The extreme heat wave in Europe in 2003 led to numerous epidemiological
studies. Reports from France (Fouillet et al., 2008) concluded that most
of the extra deaths occurred in elderly people (80% of those who died
were older than 75 years). Questions were raised at the time as to why
this event had such a devastating effect (Kosatsky, 2005). It is still not
clear, but one contributing factor may have been the relatively mild
influenza season the year before. Recent studies have found that when
the previous year’s winter mortality is low, the effect of summer heat is
increased (Rocklov and Forsberg, 2009; Ha et al., 2011) because mild
winters may leave a higher proportion of vulnerable people (Stafoggia
et al., 2009). Most studies of heat have been in high-income countries,
but there has been work recently in low- and middle-income countries,
suggesting heterogeneity in vulnerability by age groups and socioeconomic
factors similar to that seen in higher-income settings (Bell et al., 2008b;
McMichael et al., 2008; Pudpong and Hajat, 2011).
Numerous studies of temperature-related morbidity, based on hospital
admissions or emergency presentations, have reported increases in
events due to cardiovascular, respiratory, and kidney diseases (Hansen
et al., 2008; Knowlton et al., 2009; Lin and Chan, 2009) and the impact
has been related to the duration and intensity of heat (Nitschke et al.,
2011).
There is evidence now that both average levels and variability in
temperature are important influences on human health. The standard
deviation of summer temperatures was associated with survival time
in a U.S. cohort study of persons aged older than 65 years with chronic
disease who were tracked from 1985 to 2006 (Zanobetti et al., 2012).
Greater variability was associated with reduced survival. A study that
modeled separately projected increases in temperature variability and
average temperatures for six cities for 2070–2099 found that, with one
exception, variability had an effect (increased deaths) over and above
what was estimated from the rise in average temperatures (Gosling et
al., 2009). Relevant to Section 11.5, rapid changes in temperature may
also alter the balance between humans and parasites, increasing
opportunities for new and resurgent diseases. The speed with which
organisms adapt to changes in temperatures is, broadly speaking, a
function of mass, and laboratory studies have shown that microbes
respond more quickly to a highly variable climate than do their multi-
cellular hosts (Raffel et al., 2012).
Health risks during heat extremes are greater in people who are physically
active (e.g., manual laborers). This has importance for recreational
activity outdoors and it is relevant especially to the impacts of climate
change on occupational health (Kjellstrom et al., 2009a; Ebi and Mills,
2013; see also Section 11.6.2).
Heat also acts on human health through its effects, in conjunction with
low rainfall, on fire risk. In Australia in 2009, record high temperatures,
combined with long-term drought, caused fires of unprecedented
intensity and 173 deaths from burns and injury (Teague et al., 2010).
S
moke from forest fires has been linked elsewhere with increased
mortality and morbidity (Analitis et al., 2012; see Section 11.5.3.2).
11.4.1.2. Near-Term Future
The climate change scenarios modeled by WGI AR5 project rising
temperatures and an increase in frequency and intensity of heat waves
(Section 2.6.1; Chapter 1) in the near-term future, defined as roughly
midway through the 21st century, or the era of climate responsibility
(see SPM). It is uncertain how much acclimatization may mitigate the
effects on human health (Wilkinson et al., 2007a; Bi and Parton, 2008;
Baccini et al., 2011; Hanna et al., 2011; Maloney and Forbes, 2011; Peng
et al., 2011; Honda et al., 2013). In New York, it was estimated that
acclimatization may reduce the impact of added summer heat in the
2050s by roughly a quarter (Knowlton et al., 2007). In Australia, the
number of “dangerously hot” days, when core body temperatures may
increase by ≥2°C and outdoor activity is hazardous, is projected to rise
from the current 4 to 6 days per year to 33 to 45 days per year by 2070
(with SRES A1FI) for non-acclimatized people. Among acclimatized
people, an increase from 1 to 5 days per year to 5 to 14 days per year
is expected (Hanna et al., 2011).
For reasons given above, it is not clear whether winter mortality will
decrease in a warmer, but more variable, climate (Kinney et al., 2012;
Ebi and Mills, 2013). Overall, we conclude that the increase in heat-
related mortality by mid-century will outweigh gains due to fewer cold
periods, especially in tropical developing countries with limited adaptive
capacities and large exposed populations (Wilkinson et al., 2007b). A
similar pattern has been projected for temperate zones. A study of three
Quebec cities, based on SRES A2 and B2, extended to 2099, showed an
increase in summer mortality that clearly outweighed a small reduction
in autumn deaths, and only slight variations in winter and spring (Doyon
et al., 2008). Another study in Brisbane, Australia, using years of life lost
as the outcome, found the gains associated with fewer cold days were
less than the losses caused by more hot days, when warming exceeded
2°C (Huang et al., 2012).
11.4.2. Floods and Storms
Floods are the most frequently occurring type of natural disaster (Guha-
Sapir et al., 2011). In 2011, 6 of the 10 biggest natural disasters were
flood events, when considered in terms of both number affected (112
million people) and number of deaths (3140 people) (Guha-Sapir et al.,
2011). Globally, the frequency of river flood events has been increasing,
as well as economic losses, due to the expansion of population and
property in flood plains (Chapter 18). There is little information on
health trends attributable to flooding, except for mortality and there
are large differences in mortality risk between countries (UNISDR, 2011).
Mortality from flooding and storm events is generally declining, but
there is good evidence that mortality risks first increase with economic
development before declining (De Haen and Hemrich, 2007; Kellenberg
and Mobarak, 2008; Patt et al., 2010). For instance, migration to slums
in coastal cities may increase population exposure at a greater pace
than can be compensated for by mitigation measures (see Chapter 10
on urban risks). Severe damaging floods in Australia in 2010–2011 and

722
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
i
n the northeastern USA in 2012 indicate that high-income countries
may still be affected (Guha-Sapir et al., 2011).
11.4.2.1. Mechanisms
Flooding and windstorms adversely affect health through drowning,
injuries, hypothermia, and infectious diseases (e.g., diarrheal disease,
leptospirosis, vector-borne disease, cholera; Schnitzler et al., 2007;
Jakubicka et al., 2010). Since AR4, more evidence has emerged on the
long-term (months to years) implications of flooding for health. Flooding
and storms may have profound effects on peoples’ mental health (Neria,
2012). The prevalence of mental health symptoms (psychological distress,
anxiety, and depression) was two to five times higher among individuals
who reported flood water in the home compared to non-flooded
individuals (2007 flood in England and Wales; Paranjothy et al., 2011).
In the USA, signs of hurricane-related mental illness were observed in
a follow-up of New Orleans’ residents almost 2 years after Hurricane
Katrina (Kessler et al., 2008). The attribution of deaths to flood events
is complex; most reports of flood deaths include only immediate
traumatic deaths, which means that the total mortality burden is under-
reported (Health Protection Agency, 2012). There is some uncertainty
as to whether flood events are associated with a longer-term (6 to 12
months) effect on mortality in the flooded population. No persisting
effects were observed in a study in England and Wales (Milojevic et al.,
2011), but longer-term increases in mortality were found in a rural
population in Bangladesh (Milojevic et al., 2012).
11.4.2.2. Near-Term Future
Under most climate change scenarios, it is expected that more frequent
intense rainfall events will occur in most parts of the world in the future
(IPCC, 2012). If this happens, floods in small catchments will be more
frequent, but the consequence is uncertain in larger catchments (see
Chapter 3). In terms of exposure, it is expected that more people will
be exposed to floods in Asia, Africa, and Central and South America
(Chapter 3). Also, increases in intense tropical cyclones are likely in the
late 21st century (WGI AR5 Table SPM.1). It has been estimated
conservatively that around 2.8 billion people were affected by floods
between 1980 and 2009, with more than 500,000 deaths (Doocy et al.,
2013). On this basis we conclude it is very likely that health losses
caused by storms and floods will increase this century if no adaptation
measures are taken. What is not clear is how much of this projected
increase can be attributed to climate change. Dasgupta et al. (2009)
developed a spatially explicit mortality model for 84 developing countries
and 577 coastal cities. They modeled 1-in-100 year storm-surge events,
and assessed future impacts under climate change, accounting for sea
level rise and a 10% increase in event intensity. In the 84 developing
countries, an additional 52 million people and 30,000 km
2
of land were
projected to be affected by 2100.
11.4.3. Ultraviolet Radiation
Ambient ultraviolet (UV) levels and maximum summertime day
temperatures are related to the prevalence of non-melanoma skin
c
ancers and cataracts in the eye. In one study in the USA, the number
of cases of squamous cell carcinoma was 5.5% higher for every 1°C
increment in average temperatures, and basal cell carcinoma was 2.9%
more common with every 1°C increase. These values correspond to an
increase in the effective UV dose of 2% for each 1°C (van der Leun et al.,
2008). However, exposure to the sun has beneficial effects on synthesis
of vitamin D, with important consequences for health. Accordingly the
balance of gains and losses due to increased UV exposures vary with
location, intensity of exposure, and other factors (such as diet) that
influence vitamin D levels (Lucas et al., 2013). Studies of stratospheric
ozone recovery and climate change project that ultraviolet radiation
levels at the Earth’s surface will generally return to pre-1980 levels by
mid-century, and may diminish further by 2100, although there is high
uncertainty around the projections (Correa et al., 2013). On the other
hand, higher temperatures in countries with temperate climates may
result in an increase in the time which people spend outdoors (Bélanger
et al., 2009) and lead to additional UV-induced adverse effects.
11.5. Ecosystem-Mediated Impacts
of Climate Change on Health Outcomes
11.5.1. Vector-Borne and Other Infectious Diseases
Vector-borne diseases (VBDs) refer most commonly to infections
transmitted by the bite of blood-sucking arthropods such as mosquitoes
or ticks. These are some of the best-studied diseases associated with
climate change, due to their widespread occurrence and sensitivity to
climatic factors (Bangs et al., 2006; Bi et al., 2007; Halide and Ridd,
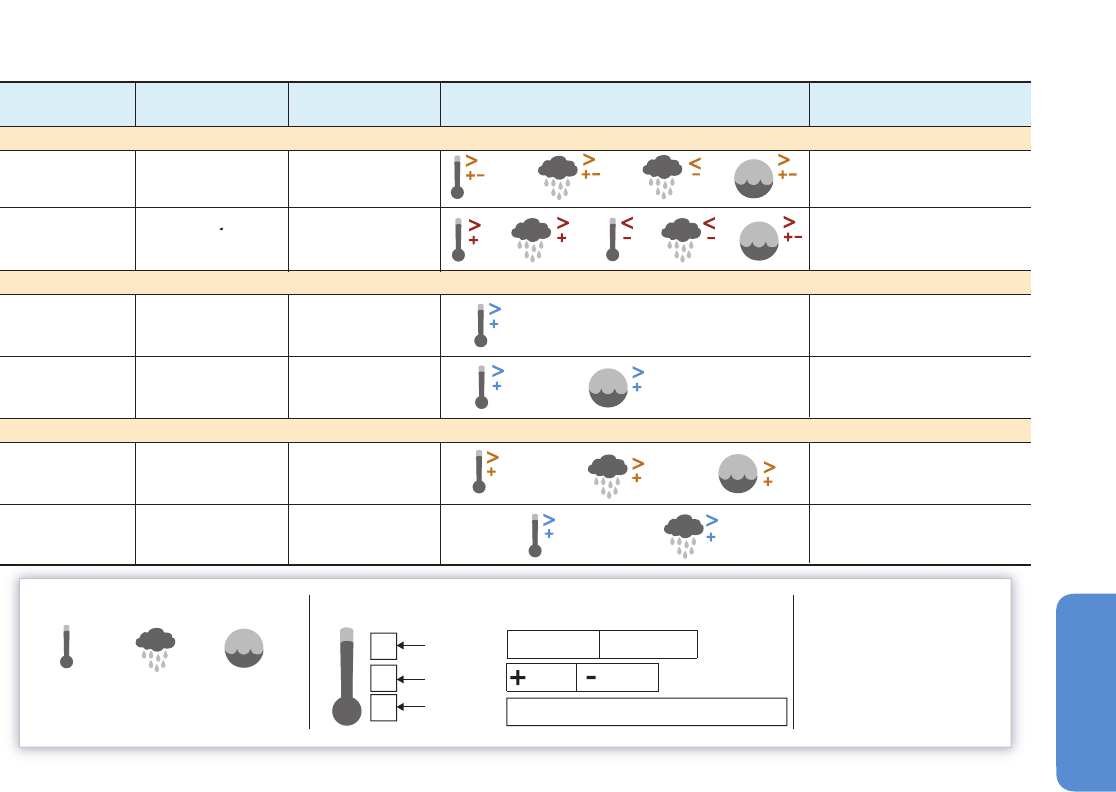
2008; Wu et al., 2009). Table 11-1 summarizes what is known about the
influence of weather and climate on selected VBDs.
11.5.1.1. Malaria
Malaria is mainly caused by five distinct species of plasmodium parasite
(Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae,
Plasmodium ovale, Plasmodium knowlesi), transmitted by Anopheline
mosquitoes between individuals. In 2010 there were an estimated 216
million episodes of malaria worldwide, mostly among children younger
than 5 years in the African Region (WHO, 2010). The number of global
malaria deaths was estimated to be 1,238,000 in 2010 (Murray et al.,
2012). Worldwide, there have been significant advances made in malaria
control in the last 20 years (Feachem et al., 2010).
The influence of temperature on malaria development appears to be
nonlinear, and is vector specific (Alonso et al., 2011). Increased variations
in temperature, when the maximum is close to the upper limit for vector
and pathogen, tend to reduce transmission, while increased variations
of mean daily temperature near the minimum boundary increase
transmission (Paaijmans et al., 2010). Analysis of environmental factors
associated with the malaria vectors Anopheles gambiae and A. funestus
in Kenya found that abundance, distribution, and disease transmission
are affected in different ways by precipitation and temperature (Kelly-
Hope et al., 2009). There are lag times according to the lifecycle of the
vector and the parasite: a study in central China reported that malaria
incidence was related to the average monthly temperature, the average
723
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
temperature of the previous 2 months, and the average rainfall of the
current month (Zhou et al., 2010).
More work has been done since AR4 to elucidate the role of local
warming on malaria transmission in the East African highlands, but this
is hampered by the lack of time series data on levels of drug resistance
and intensity of vector control programs. Earlier research had failed to
find a clear increase in temperatures accompanying increases in malaria
transmission, but new studies with aggregated meteorological data
over longer periods have confirmed increasing temperatures since 1979
(Omumbo et al., 2011; Stern et al., 2011). The strongly nonlinear response
to temperature means that even modest warming may drive large
increases in transmission of malaria, if conditions are otherwise suitable
(Pascual et al., 2006; Alonso et al., 2011). On the other hand, at relatively
high temperatures modest warming may reduce the potential of malaria
transmission (Lunde et al., 2013). One review (Chaves and Koenraadt,
2010) concluded that decadal temperature changes have played a role
in changing malaria incidence in East Africa. But malaria is very sensitive
also to socioeconomic factors and health interventions, and the generally
more conducive climate conditions have been offset by more effective
disease control activities. The incidence of malaria has reduced over
much of East Africa (Stern et al., 2011), although increased variability
in disease rates has been observed in some high-altitude areas (Chaves
et al., 2012).
At the global level, economic development and control interventions
have dominated changes in the extent and endemicity of malaria over
the last 100 years (Gething et al., 2010). Although modest warming has
facilitated malaria transmission (Pascual et al., 2006; Alonso et al.,
2011), the proportion of the world’s population affected by the disease
has been reduced, largely due to control of P. vivax malaria in moderate
climates with low transmission intensity. However, the burden of disease
is still high and may actually be on the increase again, in some locations
(WHO, 2012). For instance, locally transmitted malaria has re-emerged
in Greece in association with economic hardship and cutbacks in
government spending (Danis et al., 2011; Andriopoulos et al., 2013).
11.5.1.2. Dengue Fever
Dengue is the most rapidly spreading mosquito-borne viral disease,
showing a 30-fold increase in global incidence over the past 50 years
(WHO, 2013). Each year there occur about 390 million dengue infections
worldwide, of which roughly 96 million manifest with symptoms (Bhatt
et al., 2013). Three quarters of the people exposed to dengue are in the
Asia-Pacific region, but many other regions are affected also. The first
sustained transmission of dengue in Europe since the 1920s was
reported in 2012 in Madeira, Portugal (Sousa et al., 2012). The disease
is associated with climate on spatial (Beebe et al., 2009; Russell et al.,
Other vector-borne diseases
Hemorrhagic fever
with renal
syndrome (HFRS)
Plague
Disease
Area Cases per year Key references
Mainly Africa, SE Asia
100 countries,
esp. Asia Pacific
Tick-borne diseases
Climate sensitivity and
confidence in climate effect
WHO (2008); Kelly-Hope et al.
(2009); Alonso et al. (2011);
Omumbo et al. (2011)
Lyme
Tick-borne
encephalitis
Dengue
Malaria
Beebe (2009); Pham et al. (2011);
Astrom et al. (2012); Earnest et
al. (2012); Descloux (2012)
About 220 million
About 50 million
About 10,000
About 20,000 in USA
0.15–0.2 million
About 40,000
Europe, Russian Fed.,
Mongolia, China
Temperate areas of
Europe, Asia, North
America
Global
Endemic in many
locations worldwide
Tokarevich et al. (2011)
Bennet (2006); Ogden et al. (2008)
Fang et al. (2010)
Stenseth et al. (2006); Ari et al.
(2010); Xu et al. (2011)
Climate drivers Climate driver variables Confidence levels
Temperature Precipitation
Humidity
High confidence in global effect
High confidence in local effect
Low confidence in effect
1
1
%
%
%
%
%
Footnote
Increase or
decrease
# of cases
More
Fewer
Increased Decreased
>>
<<
Mosquito-borne diseases
1 Effects are specific to Anopheles spp
Table 11-1 | The association between different climatic drivers and the global prevalence and geographic distribution of selected vector-borne diseases observed over the period
2008-2012. Among the vector-borne diseases shown here, only dengue fever was associated with climate variables at both the global and local levels (high confidence), while
malaria and hemorrhagic fever with renal syndrome showed a positive association at the local level (high confidence).
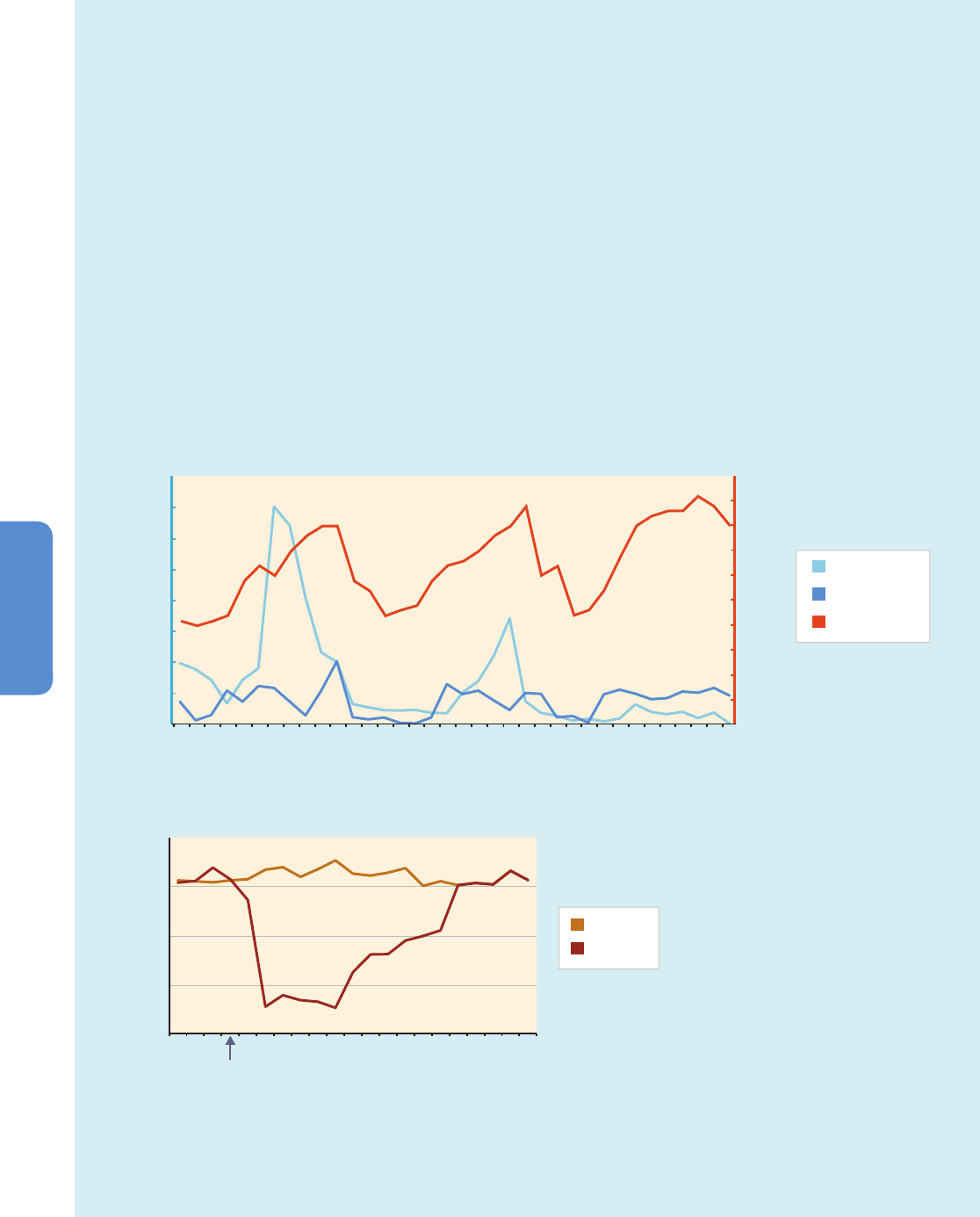
724
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Box 11-2 | Case Study: An Intervention to Control Dengue Fever
Seasonality in dengue transmission is well established in many parts of the world, and transmission occurs mostly during the wettest
months of the year (Gubler and Kuno, 1997; Chadee et al., 2007). Figure 11-3 shows that about 80% of dengue fever cases in
Trinidad were recorded during the wet season, a period when the Ae. aegypti mosquito population density was four to nine times
higher than the dengue transmission threshold (Macdonald, 1956). This led to a control program that concentrated on reducing the
mosquito population before the onset of the rains, by application of insecticides (temephos) into the water drums that serve as primary
breeding sites of Ae. aegypti in the Caribbean. The one-off treatment effectively controlled the mosquito populations for almost 12
weeks after which the numbers reverted to levels observed in the untreated control areas.
Climate scenarios that extend to 2071–2100 project changes in the intensity and frequency of rainfall events in the Caribbean
(Campbell et al., 2011). In these scenarios, there is greater variability in rainfall patterns during November to January, with the northern
Caribbean region receiving more rainfall than in the southern Caribbean (Campbell et al., 2011). There may be water shortages during
drought periods, and flooding after episodes of heavy rainfall, both of which affect the breeding habitats of Ae. aegypti and Ae.
albopictus. Vector control strategies will need to be planned and managed astutely to systematically reduce mosquito populations.
0
500
1000
1500
2000
1357911 13 15 17 19 21
(b) Efficacy of pre-seasonal treatment with temephos on Aedes aegypti ovitrap egg counts in Curepe (treatment) and St. Joseph (control),
Trinidad (2003)
(a) Rainfall, Breteau index, and Dengue cases, Trinidad (2002–2004)
Weeks
Number of eggs
Breteau
Dengue cases
Rainfall (mm)
0
200
400
600
800
1000
1200
1400
1600
M
arc
h
Ju
ly
S
e
p
t
N
o
v
M
a
rc
h
Ju
ly
S
ept
N
ov
Ma
rc
h
Jul
y
Se
p
t
No
v
Breteau index
Number of dengue cases/
Rainfall (mm)
Control
Treatment
Figure 11-3 | (a) Rainfall, Breteau index (number of water containers with Ae. aegypti larvae per 100 houses), and dengue fever cases, Trinidad (2002–2004). Rainfall
was found to be significantly correlated with an increase in the Ae. aegypti population and dengue fever incidence, with a clearly defined “dengue season” between
June and November over two years of the study (Chadee et al., 2007). b) Efficacy of pre-seasonal treatment with temephos on Ae. aegypti ovitrap egg counts in Curepe
(treatment) and St. Joseph (control), Trinidad (2003). Evidence of the efficacy of the pre-seasonal larval control through focal treatment of Ae. aegypti population is
provided. Treatment at the onset of the rainy season can effectively prevent the rapid increase in Ae. aegypti populations and therefore suppress the onset of dengue
transmission (Chadee, 2009).
0
5
10
15
20
30
35
40
50
25
45
Rains start

725
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
2
009; Li et al., 2011), temporal (Hii et al., 2009; Hsieh and Chen, 2009;
Herrera-Martinez and Rodriguez-Morales, 2010; Gharbi et al., 2011; Pham
et al., 2011; Descloux et al., 2012; Earnest et al., 2012) and spatiotemporal
(Chowell et al., 2008, 2011; Lai, 2011) scales.
The principal vectors for dengue, Aedes aegypti and Ae. albopictus, are
climate sensitive. Over the last 2 decades, climate conditions have
become more suitable for albopictus in some areas (e.g., over
central northwestern Europe) but less suitable elsewhere (e.g., over
southern Spain) (Caminade et al., 2012). Distribution of Ae. albopictus
in northwestern China is highly correlated with annual temperature and
precipitation (Wu et al., 2011). Temperature, humidity, and rainfall are
positively associated with dengue incidence in Guangzhou, China, and
wind velocity is inversely associated with rates of the disease (Lu and
Lin, 2009; Li et al., 2011). Several studies in Taiwan reported that
typhoons remain an important factor affecting vector population and
dengue fever (Hsieh and Chen, 2009; Lai, 2011). Typhoons result in
extreme rainfall, high humidity, and water pooling, and may generate
fresh mosquito breeding sites. A study in Dhaka, Bangladesh, reported
increased rates of admissions to hospital due to dengue with both
high and low river levels (Hashizume and Dewan, 2012). In some
circumstances, it is apparent that heavy precipitation favors the spread
of dengue fever, but drought can also be a cause if households store
water in containers that provide suitable mosquito breeding sites
(Beebe et al., 2009; Padmanabha et al., 2010).
11.5.1.3. Tick-Borne Diseases
Tick-borne encephalitis (TBE) is caused by tick-borne encephalitis virus,
and is endemic in temperate regions of Europe and Asia. Lyme disease is
an acute infectious disease caused by the spirochaete bacteria Borrelia
burgdorferi and is reported in Europe, the USA, and Canada. Borrelia is
transmitted to humans by the bite of infected ticks belonging to a few
species of the genus Ixodes (“hard ticks”). Many studies have reported
associations between climate and tick-borne diseases (Okuthe and Buyu,
2006; Lukan et al., 2010; Tokarevich et al., 2011; Andreassen et al., 2012;
Estrada-Peña et al., 2012; Jaenson et al., 2012). In North America, there
is good evidence of northward expansion of the distribution of the tick
vector (Ixodes scapularis) in the period 1996–2004 based on an analysis
of active and passive surveillance data (Ogden et al., 2010). However,
there is no evidence so far of any associated changes in the distribution
in North America of human cases of tick-borne diseases.
There was a marked rise in TBE cases from the 1970s in central and
Eastern Europe. Spring-time daily maximum temperatures rose in the
late 1980s, sufficient to encourage transmission of the TBE virus. For
instance, in the Czech Republic, between 1970 and 2008, there were
signs of lengthening transmission season and higher altitudinal range
in association with warming (Kriz et al., 2012). However variations in
illness rates across the region demonstrate that climate change alone
cannot explain the increase. Socioeconomic changes (including changes
in agriculture and recreational activities) have affected patterns of disease
in Europe (Sumilo et al., 2008; Randolph, 2010). The complex ecology
of tick-borne diseases such as Lyme disease and TBE make it difficult to
attribute particular changes in disease frequency and distribution to
specific environmental factors such as climate (Gray et al., 2009).
11.5.1.4. Other Vector-Borne Diseases
Hemorrhagic fever with renal syndrome (HFRS) is a zoonosis caused by
the Hanta virus, and leads to approximately 200,000 hospitalized cases
each year. The incidence of this disease has been associated with
temperature, precipitation, and relative humidity (Pettersson et al., 2008;
Fang et al., 2010; Liu et al., 2011). Plague, one of the oldest diseases
known to humanity, persists in many parts of the world. Outbreaks have
been linked to seasonal and interannual variability in climate (Stenseth
et al., 2006; Nakazawa et al., 2007; Holt et al., 2009; Xu et al., 2011;
MacMillan et al., 2012). Chikungunya fever is a climate-sensitive mosquito-
transmitted viral disease (Anyamba et al., 2012), first identified in Africa,
now present also in Asia, and the disease has recently emerged in parts
of Europe (Angelini et al., 2008). The incidence in China of Japanese
encephalitis, another mosquito-borne viral disease, is correlated with
temperature and rainfall, especially during the warmer months of the
year (Bai et al., 2013). In West Africa, outbreaks of Rift Valley Fever, an
acute viral disease affecting humans and domestic animals, are linked
to within-season variability in rainfall (Caminade et al., 2011).
11.5.1.5. Near-Term Future
Using the A1B climate change scenario, Béguin et al. (2011) projected
the population at risk of malaria to 2030 and 2050. With GDP per capita
held constant at 2010 values, the model projected 5.2 billion people at
risk in 2050, out of a predicted global population of 8.5 billion. Keeping
climate constant, and assuming strong economic growth allied with
social development (“best case”), the model projected 1.74 billion
people at risk (approximately half the present number at risk) in 2050.
Factoring in climate change would increase the “best case” estimate
of the number of people at risk of malaria in 2050 to 1.95 billion, which
is 200 million more than if disease control efforts were not opposed by
higher temperatures and shifts in rainfall patterns.
There are no recent studies that project the return of established malaria
to North America or Europe, where it was once prevalent. However,
suitable vectors for P. vivax malaria abound in these parts of the world,
and recent experience in southern Europe demonstrates how rapidly
the disease may reappear if health services falter (Bonovas and
Nikolopoulos, 2012).
A systematic review of research on the distribution of dengue and
possible influence of climate change (Van Kleef et al., 2010) concluded
that the area of the planet that was climatically suitable for dengue
would increase under most scenarios, but it was not possible to project
the impact on disease incidence. Åström et al. (2012) estimated the
population at risk out to the year 2050. The study was based on routine
disease reports, surveys, population projections, estimates of GDP
growth, and the A1B scenario for climate change. Assuming high GDP
growth that benefits all populations, the number exposed to dengue in
2050 falls to 4.46 billion; that is, the adverse effects of climate change
are balanced by the beneficial outcomes of development. This study
considered only the margins of the geographic distribution of dengue
(where economic development has its strongest effect) and did not
examine changes in intensity of transmission in areas where the disease
is already established.

726
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
K
earney (2009) used biophysical models to examine the potential
extension of vector range in Australia. He predicted that climate change
would increase habitat suitability throughout much of Australia.
Changes in water storage as a response to a drier climate may be an
indirect pathway, through which climate change affects mosquito
breeding (Beebe et al., 2009).
11.5.2. Food- and Water-Borne Infections
Human exposure to climate-sensitive pathogens occurs by ingestion of
contaminated water or food; incidental ingestion during swimming; or
by direct contact with eyes, ears, or open wounds. Pathogens in water
may be zoonotic in origin, concentrated by bivalve shellfish (e.g., oysters),
or deposited on irrigated food crops. Pathogens of concern include
enteric organisms that are transmitted by the fecal oral route and also
bacteria and protozoa that occur naturally in aquatic systems. Climate
may act directly by influencing growth, survival, persistence, transmission,
or virulence of pathogens; indirect influences include climate-related
perturbations in local ecosystems or the habitat of species that act as
zoonotic reservoirs.
11.5.2.1. Vibrios
Vibrio is a genus of native marine bacteria that includes a number of
human pathogens, most notably V. cholerae which causes cholera.
Cholera may be transmitted by drinking water or by environmental
exposure in seawater and seafood; other Vibrio species are solely
linked to seawater and shellfish. These include V. parahaemolyticus and
V. vulnificus, with V. alginolyticus emerging in importance (Weis, 2011).
Risk of infection is influenced by temperature, precipitation, and
accompanying changes in salinity due to freshwater runoff, addition of
organic carbon or other nutrients, or changes in pH. These factors all
affect the spatial and temporal range of the organism and also influence
exposure routes (e.g., direct contact or via seafood). In countries with
endemic cholera, there appears to be a robust relationship between
temperature and the disease (Islam, 2009; Paz, 2009; Reyburn et al., 2011).
In addition, heavy rainfall promotes the transmission of pathogens when
there is not secure disposal of fecal waste. An unequivocal positive
relationship between Vibrio numbers and sea surface temperature in
the North Sea has been established by DNA analyses of formalin-fixed
samples collected over a 44-year period (Vezzulli et al., 2012). Cholera
outbreaks have been linked to variations in temperature and rainfall,
and other variables including sea and river levels, sea chlorophyll and
cyanobacteria contents, and Indian Ocean Dipole (IOD) and El Niño-
Southern Oscillation (ENSO) events (de Magny et al., 2008; Hashizume,
2008; Bompangue et al., 2011; Reyburn et al., 2011; Rinaldo et al., 2012).
11.5.2.2. Other Parasites, Bacteria, and Viruses
Rates of diarrhea have been associated with high temperatures (Kolstad
and Johansson, 2011). Mostly, however, neither the specific causes of
the diarrheal illness are known, nor the mechanism for the association
with temperature. Exceptions include Salmonella and Campylobacter,
among the most common zoonotic food- and water-borne bacterial
p
athogens worldwide, which both show distinct seasonality in infection
and higher disease rates at warmer temperatures. The association
between climate (especially temperature) and non-outbreak (“sporadic”)
cases of salmonellosis may, in part, explain seasonal and latitudinal
trends in diarrhea (Lake, 2009).
Among the enteric viruses, there are distinct seasonal patterns in infection
that can be related indirectly to temperature. Enterovirus infections in
the USA peak in summer and fall months (Khetsuriani et al., 2006). After
controlling for seasonality and interannual variations, hand, foot, and
mouth disease (caused by coxsackievirus A16 and enterovirus 71) shows
a linear relationship with temperature in Singapore, with a rapid rise in
incidence when the temperature exceeds 32°C (Hii et al., 2011). However,
it is not clear what the underlying driver is and if temperature is
confounded by other seasonal factors.
Temperature is directly linked with risk of enteric disease in Arctic
communities, as melt of the permafrost hastens transport of sewage
(which is often captured in shallow lagoons) into groundwater,
drinking water sources, or other surface waters (Martin et al., 2007). In
addition, thawing may damage drinking water intake systems (for those
communities with such infrastructure) (Hess, 2008).
Rainfall has also been associated with enteric infections. Bacterial
pathogens are more likely to grow on produce crops (e.g., lettuce) in
simulations of warmer conditions (Liu et al., 2013a), and become
attached to leafy crops under conditions of both flooding and drought
(Ge et al., 2012). This latter pattern is reflected in patterns of illness
(Bandyopadhyay et al., 2012). Higher concentrations of enteric viruses
have been reported frequently in drinking water and recreational water
following heavy rainfall (Delpla et al., 2009).
Worldwide, rotavirus infections caused about 450,000 deaths in children
younger than 5 years old in 2008 (Tate et al., 2012). There are seasonal
peaks in the number of cases in temperate and subtropical regions but
less distinct patterns are seen within 10° latitude of the equator (Cook et
al., 1990). Variations in the timing of peak outbreaks between countries
or regions (Turcios et al., 2006; Atchison et al., 2010) and variations with
time in the same country (Dey et al., 2010) have been attributed to
fluctuations in the number and seasonality of births (Pitzer et al., 2009,
2011). While vaccination against rotavirus is expected to reduce the
total burden of disease, it may also increase seasonal variation (Tate et
al., 2009; Pitzer et al., 2011).
Harmful algal blooms can be formed by (1) dinoflagellates that cause
outbreaks of paralytic shellfish poisoning, ciguatera fish poisoning, and
neurotoxic shellfish poisoning; (2) cyanobacteria that produce toxins
causing liver, neurological, digestive, and skin diseases; and (3) diatoms
that can produce domoic acid, a potent neurotoxin that is bioaccumulated
in shellfish and finfish (Erdner et al., 2008). Increasing temperatures
promote bloom formation in both freshwater (Paerl et al., 2011) and
marine environments (Marques et al., 2010; see Chapter 5). Increasing
temperature favored growth of toxic over non-toxic strains of Microcystis
in lakes in the USA (Davis et al., 2009). Projections of toxin-producing
blooms in Puget Sound using an A1B scenario suggest that by the end
of the century the “at risk” period may begin 2 months earlier and last
up to 1 month longer than at present (Moore et al., 2011).
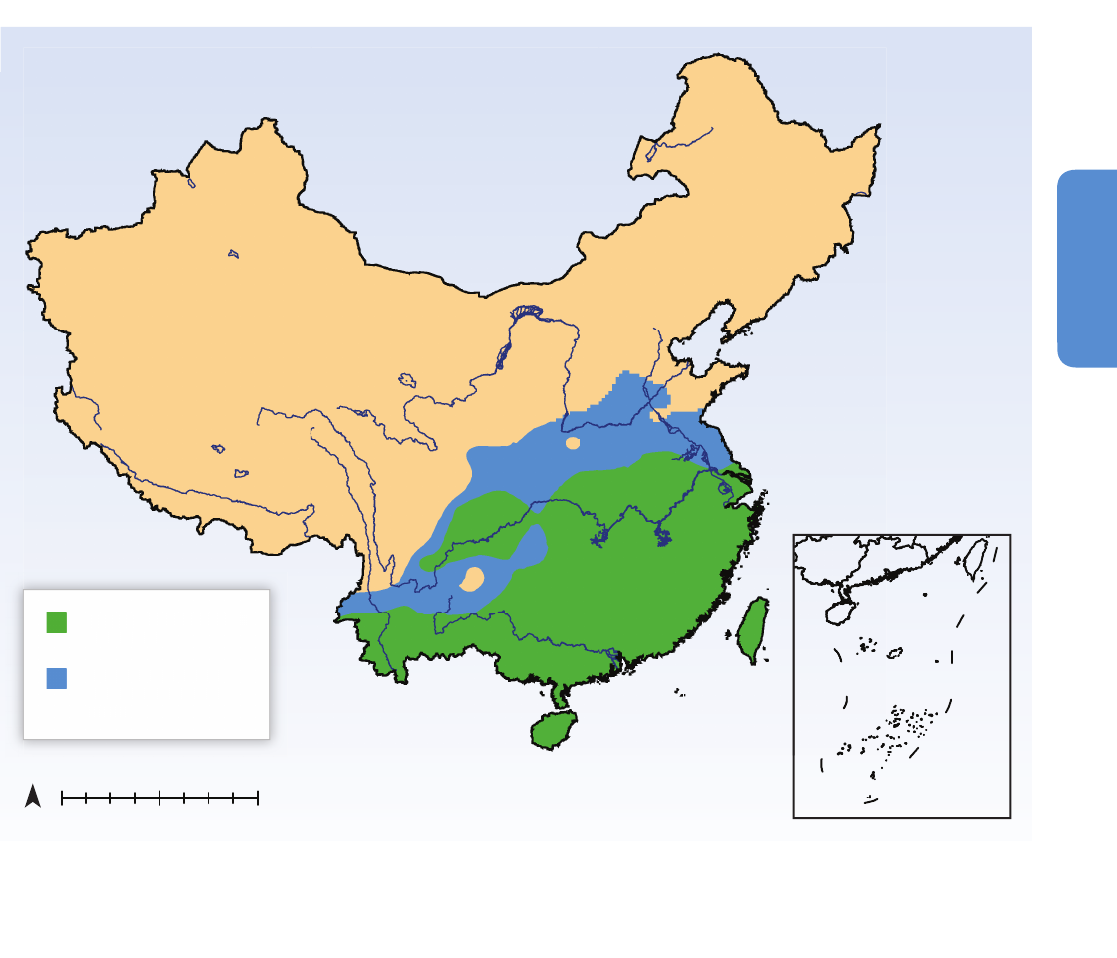
727
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
11.5.2.3. Near-Term Future
Kolstad and Johansson (2011) projected an increase of 8 to 11% in the
risk of diarrhea in the tropics and subtropics in 2039 due to climate
change, using the A1B scenario and 19 coupled atmosphere-ocean
climate models from CMIP3. This study did not account for future
changes in economic growth and social development. Application of
down-scaled climate change models showed that overflows of sewage
into Chicago’s watersheds would increase by 50 to 120% by 2100, as
a result of more frequent and intense rainfall (Patz et al., 2008). In
Botswana, if hot, dry conditions begin earlier in the year, and are
prolonged, as projected by down-scaled climate scenarios, the present
dry season peak in diarrheal disease may be amplified (Alexander et
al., 2013). However, the same analysis projected that incidence of
diarrheal disease in the wet season would decline. Zhou et al. (2008)
studied the effect of climate on transmission of schistosomiasis due to
S. japonicum in China. They concluded that an additional 784,000 km
2
w
ould become suitable for schistosomiasis transmission in China by
2050, as the mid-winter freezing line moves northward (Figure 11-4).
Mangal et al. (2008) constructed a mechanistic model of the transmission
cycle of another species, S. mansoni, and reported a peak in the worm
burden in humans at an ambient temperature of 30°C, falling sharply
as temperature rises to 35°C. The authors attribute this to the increasing
mortality of both the snails and the water-borne intermediate forms of
the parasite, and noted that worm burden is not directly linked to the
prevalence of schistosomiasis.
11.5.3. Air Quality
Nearly all the non-CO
2
climate-altering pollutants (see WGI AR5 Chapters
7 and 8) are health damaging, either directly or by contributing to
secondary pollutants in the atmosphere. Thus, like the ocean acidification
250 500 1000 km0
N
Range of schistosomiasis in
China in 2000
Additional area suitable
for disease transmission
in 2050
Range of
schistosomiasis
in
Chi
na
in
200
0
Additional area suitable
for
di
sease transm
iss
ion
in 2050
Figure 11-4 | Effect of rising temperatures on the area in which transmission of Schistosomiasis japonica may occur. Green area denotes the range of schistosomiasis in China in
2000. The blue area shows the additional area suitable for disease transmission in 2050. Based on a biology-driven model including parasite (Schistosoma japonicum) and snail
intermediate host (Oncomelania hupensis) and assuming average temperatures in China in mid-winter (January) increase by 1.6°C in 2050, compared with 2000 (adapted from
Zhou et al., 2008).
728
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
and ecosystem/agriculture fertilization impacts of CO
2
, the other CAPs
have non-climate-mediated impacts, particularly on health. Although
not reviewed in detail in this assessment, the health impacts of non-
CO
2
CAPs are substantial globally. See Box 11-3.
Although there is a large body of literature on the health effects of
particulate air pollution (see Box 11-3), WGI indicates that there is little
evidence that climate change, per se, will affect long-term particle levels
in a consistent way (WGI AR5 Section 11.3.5 and Annex II). Thus, we
focus here on chronic ozone exposures, which are found by WGI to be
enhanced in some, but not all, scenarios of future climate change
(WGI AR5 TS.5.4.8).
11.5.3.1. Long-Term Outdoor Ozone Exposures
Tropospheric ozone is formed through photochemical reactions that
involve nitrogen oxides (NO
x
), carbon monoxide (CO), methane (CH
4
),
and volatile organic compounds (VOCs) in the presence of sunlight and
elevated temperatures (WGI AR5 Chapter 8). Therefore, if temperatures
Box 11-3 | Health and Economic Impacts of Climate-Altering Pollutants Other than CO
2
Although other estimates of the global health impacts of human exposures to particle and ozone pollution have been published in
recent years (e.g., UNEP, 2011), the most comprehensive was the Comparative Risk Assessment carried out as part of the 2010
Global Burden of Disease Project (Lim et al., 2012). It found that the combined health impact of the household exposures to particle
air pollution from poor combustion of solid cooking fuels, plus general ambient pollution, was about 6.8 million premature deaths
annually, with about 5% overlapping, that is, coming from the contribution to general ambient pollution of household fuels. It also
found that about 150,000 premature deaths could be attributed to ambient ozone pollution. Put into terms of disability-adjusted life
years (DALYs), particle air pollution was responsible for about 190 million lost DALYs in 2010, or about 7.6% of all DALYs lost. This
burden puts particle air pollution among the largest risk factors globally, far higher than any other environmental risk and rivaling or
exceeding all of the five dozen risk factors examined, including malnutrition, smoking, high blood pressure, and alcohol.
The economic impact of this burden is difficult to assess as evaluation methods vary dramatically in the literature. Most in the health
field prefer to consider some version of a lost healthy life year as the best metric although the economics literature often uses
willingness to pay for avoiding a lost life (Jamison et al., 2006). Another difficulty is that any valuation technique that weights the
economic loss according to local incomes per capita will value health effects in rich countries more than in poor countries, which
would seem to violate some of the premises of a global assessment; see WGIII AR5 Chapter 3 for more discussion. Here, however, we
will use the mean global income per capita (approximately US$10,000 in 2010) to scope out the scale of the impact globally without
attempting to be specific by country or region.
The WHO CHOICE approach for evaluating what should be spent on health interventions indicates that one annual per capita income
per DALY is a reasonable upper bound (WHO, 2009a). This would imply that the total lost economic value from global climate-altering
pollutants in the form of particles is roughly US$1.9 trillion, in the sense that the world ought to be willing to pay this much to reduce
it. This is about 2.7% of the global economy (approximately US$70 trillion in 2010).
On the one hand, this shows that global atmospheric pollution already has a major impact on the health and economic well-being of
humanity today, due mainly to the direct effects rather than those mediated through climate. If CO
2
is not controlled and climate
change continues to intensify while air pollutant controls become more stringent, the climate impacts will become more prominent.
The quite different time scales for the two types of impacts make comparisons difficult, however.
Air pollution reductions do not always promote the twin goals of protecting health and climate but can pose trade-offs. All particles
are dangerous for health, for example, but some are cooling, such as sulfates, and some warming, such as black carbon (Smith et al.,
2009). Indeed elimination of all anthropogenic particles in the atmosphere, a major success for health, would have only a minor net
impact on climate (WGI AR5 Figure TS-6). As discussed in Section 11.9, there are nevertheless specific actions that will work toward
both goals.

729
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
r
ise, many air pollution models (Ebi and McGregor, 2008; Tsai et al.,
2008; Chang et al., 2010; Polvani et al., 2011) project increased ozone
production especially within and surrounding urban areas (Hesterberg et
al., 2009). Enhanced temperature also accelerates destruction of ozone,
and the net direct impact of climate change on ozone concentrations
worldwide is thought to be a reduction (WGI AR5 TS.5.4.8). Some WGI
(TS.5.4.8) scenarios, however, indicate tropospheric ozone may rise from
additional CH
4
emissions stimulated by climate change. Models also
show that local variations can have a different sign to the global one
(Selin et al., 2009).
Even small increases in atmospheric concentrations of ground-level
ozone may affect health (Bell et al., 2006; Ebi and McGregor, 2008;
Jerrett et al., 2009). For instance, Bell et al. (2006) found that levels that
meet the USEPA 8-hour regulation (0.08 ppm over 8 hours) were
associated with increased risk of premature mortality. There is a lack of
association between ozone and premature mortality only at very low
concentrations (from 0 to ~10 ppb) but the association becomes positive
and approximately linear at higher concentrations (Bell et al., 2006; Ebi
and McGregor, 2008; Jerrett et al., 2009). In an analysis of 66 U.S. cities
with 18 years of follow-up (1982–2000), tropospheric ozone levels were
found to be significantly associated with cardiopulmonary mortality
(Smith et al., 2009). See also the global review by WHO, which includes
data from developing countries (WHO, 2006).
11.5.3.2. Acute Air Pollution Episodes
Wildfires, which occur more commonly following heat waves and
drought, release particulate matter and other toxic substances that may
affect large numbers of people for days to months (Finlay et al., 2012;
Handmer et al., 2012). During a fire near Denver (USA) in June 2009,
1-hour concentrations of particulate matter with aerodynamic diameter
<10 μm (PM
10
) and particulate matter with aerodynamic diameter <2.5
μm (PM
2.5
) reached 370 µg m
–3
and 200 µg m
–3
, and 24-hour average
concentrations reached 91 µg m
–3
and 44 µg m
–3
(Vedal and Dutton,
2006), compared to the 24-hour WHO Air Quality Guidelines (AQGs) for
these pollutants of 50 µg m
–3
and 25 µg m
–3
, respectively. One study of
worldwide premature mortality attributable to air pollution from forest
fires estimated there were 339,000 deaths per year (range 260,000 to
600,000) (Johnston et al., 2012). The regions most affected are sub-
Saharan Africa and Southeast Asia (Johnston et al., 2012). Extremely
high levels of PM
10
were observed in Moscow due to forest fires caused
by a heat wave in 2010. Daily mean temperatures in Moscow exceeded
the respective long-term averages by 5°C or more for 45 days. Ten new
temperature records were established in July and nine in August, based
on measurements since 1885, and an anti-cyclone in the Moscow region
prevented dispersion of air pollutants. The highest 24-hour pollution
levels recorded in Moscow during these conditions were between 430
and 900 µg m
–3
PM
10
most days, but occasionally reached 1500 µg m
–3
.
The highest 24-hour CO concentration was 30 mg m
–3
compared to the
WHO AQGs of 7 mg m
–3
, and the levels of formaldehyde, ethyl benzene,
benzene, toluene, and styrene were also increased (State Environmental
Institution “Mosecomonitoring,” 2010).
There may be an interaction of tropospheric ozone and heat waves.
Dear et al. (2005) modeled the daily mortality due to heat and exposure
t
o ozone during the European summer heat wave of 2003 and found
that possibly 50% of the deaths could have been associated with ozone
exposure rather than the heat itself.
11.5.3.3. Aeroallergens
Allergic diseases are common and some are climate sensitive. Warmer
conditions generally favor the production and release of airborne
allergens (such as fungal spores and plant pollen) and, consequently,
there may be an effect on asthma and other allergic respiratory diseases
such as allergic rhinitis, as well as effects on conjunctivitis and dermatitis
(Beggs, 2010). Children are particularly susceptible to most allergic
diseases (Schmier and Ebi, 2009). Increased release of allergens may be
amplified if higher CO
2
levels stimulate plant growth. Visual monitoring
and experiments have shown that increases in air temperature cause
earlier flowering of prairie tallgrass (Sherry et al., 2007). Droughts and high
winds may produce windborne dust and other atmospheric materials,
which contain pollen and spores, and transport these allergens to new
regions.
Studies have shown that increasing concentrations of grass pollen lead
to more frequent ambulance calls due to asthma symptoms, with a time
lag of 3 to 5 days (Heguy et al., 2008). Pollen levels have also been
linked to hospital visits with rhinitis symptoms (Breton et al., 2006). A
cross-sectional study in the three climatic regions of Spain documented
a positive correlation between the rate of child eczema and humidity,
and negative correlation between child eczema and air temperature or
the number of sunshine hours (Suarez-Varela et al., 2008).
11.5.3.4. Near-Term Future
It is projected by WGI that climate change could affect future air quality,
including levels of photochemical oxidants and, with much less certainty,
fine particles (PM
2.5
). If this occurs, there will be consequences for human
health (Bell et al., 2007; Dong et al., 2011; Chang et al., 2012; Lepeule
et al., 2012; Meister et al., 2012; West et al., 2013). High temperatures
may also magnify the effects of ozone (Ren et al., 2008; Jackson et al.,
2010). Increasing urbanization, use of solid biomass fuels, and industrial
development in the absence of emission controls could also lead to
increases in ozone chemical precursors (Selin et al., 2009; Wilkinson et
al., 2009).
Most post-2006 studies on the projected impacts of future climate
change on air pollution-related morbidity and mortality have focused
on ozone in Europe, the USA, and Canada (Bell et al., 2007; Selin et al.,
2009; Tagaris et al., 2009). Projections are rare for other areas of the
world, notably the developing countries where air pollution is presently
a serious problem and is expected to worsen unless controls are
strengthened.
Higher temperatures may magnify the effects of air pollutants like
ozone, although estimates of the size of this effect vary (Ren et al., 2008;
Jackson et al., 2010). In general, all-cause mortality related to ozone is
expected to increase in the USA and Canada (Bell et al., 2007; Tagaris et
al., 2009; Jackson et al., 2010; Cheng et al., 2011). Under a scenario in
730
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
w
hich present air quality legislation is rolled out everywhere, premature
deaths due to ozone would be wound back in Africa, South Asia, and
East Asia. Under a maximum feasible CO
2
reduction scenario related to
A2, it is projected that 460,000 premature ozone-related deaths could
be avoided in 2030, mostly in South Asia (West et al., 2007a). All-cause
mortality, however, is not the best metric for comparing air pollution
health impacts across regions, given that background disease conditions
vary so widely. HIV deaths and malaria deaths, which are prominent in
sub-Saharan Africa, for example, are not expected to increase from air
pollution exposures in the same way as deaths from cardiovascular
disease that dominate other regions.
A study that investigated regional air quality in the USA in 2050, using
a down-scaled climate model (Goddard Institute for Space Studies,
Global Climate Model), concluded there would be about 4000 additional
annual premature deaths due to increased exposures to PM
2
.5
(Tagaris
et al., 2009). Air pollutant-related mortality increases are also projected
for Canada, but in this case they are largely driven by the effects of
ozone (Cheng et al., 2011). On the basis of the relation of asthma to air
quality in the last decade (1999–2010), Thompson et al. (2012) anticipate
that the prevalence of asthma in South Africa will increase substantially
by 2050. Sheffield et al. (2011), applying the SRES A2 scenario, projected
a median 7.3% increase in summer ozone-related asthma emergency
department visits for children (0 to 17 years) across New York City by
the 2020s compared to the 1990s.
11.6. Health Impacts Heavily Mediated
through Human Institutions
11.6.1. Nutrition
Nutrition is a function of agricultural production (net of post-harvest
wastes and storage losses), socioeconomic factors, such as food prices
and access, and human diseases, especially those that affect appetite,
nutrient absorption, and catabolism (Black et al., 2008; Lloyd et al.,
2011). All three may be influenced by climate but only agricultural
production has been modeled in a climate impacts framework. Here
we use the terms undernutrition, which is a health outcome, and
undernourishment, which reflects national (post-trade) calories available
for human consumption, and is expressed as estimated percent of the
population receiving “insufficient” calories. We do not use the term
“malnutrition,” as it includes overnutrition, which is not considered
here (except under co-benefits in Section 11.9). Undernutrition can be
chronic, leading to stunting (low height for age), or acute, leading to
wasting (low weight for height); underweight (low weight for age) is a
combination of chronic and acute undernutrition.
11.6.1.1. Mechanisms
The processes through which climate change can affect human nutrition
are complex (see Section 7.2.2). Higher temperatures and changes in
precipitation may reduce both the quantity and quality of food
harvested (e.g., Battisti and Naylor, 2009). Lobell et al. (2011b) showed
for African maize that for each degree above 30°C, yields decreased by
1% under optimal rainfall conditions and by 1.7 % under drought
conditions. From their systematic review of more than a thousand
studies, Knox et al. (2012) drew the conclusion that “climate change is
a threat to crop productivity in areas that are already food insecure.”
Rising temperatures may also affect food security through the impact
of heat on productivity of farmers (see Section 11.6.2).
The magnitude of detected and predicted decline in land-based
agricultural production due to increasing temperatures and changes in
rainfall must be put in perspective to other changes, such as increase
in harvests due to improved farming knowledge and technology, the
amount of food fed to livestock, used for biofuels, consumed beyond
baseline needs by the overnourished, or wasted in other ways (Foley et
al., 2011). There is good evidence that local food price increases have
negative effects on food consumption, and therefore on health (Green
et al., 2013). Against this background, the global food price fluctuates,
though with a recently rising trend. While the main driver is higher
energy costs, amplified by speculation (Piesse and Thirtle, 2009), there
is growing evidence (Auffhammer, 2011) that extreme weather events,
especially floods, droughts (Williams and Funk, 2011), and heat waves,
may have contributed to higher prices. All else being equal, higher prices
increase the number of malnourished people. See Chapter 7 for a more
detailed discussion of the impact of climate change on food production.
11.6.1.2. Near-Term Future
Since AR4 at least four studies have been published which project the
effect of climate change on undernourishment and undernutrition.
Nelson et al. (2009, 2010) conducted two studies using a crop simulation
model (DSSAT) and a global agricultural trade model (IMPACT 2009) to
estimate crop production (with and without CO
2
enrichment), calorie
availability, child underweight, and adaptation costs. The first study
(Nelson et al., 2009) was carried out under the A2 emission scenario,
using two General Circulation Models (GCMs): National Center for
Atmospheric Research (NCAR) and Commonwealth Scientific and
Industrial Research Organisation (CSIRO) and relative to a “no climate
change” future. The authors found that yields of most important crops
would decline in developing countries by 2050, that per capita calorie
Scenario South Asia East Asia / Pacifi c
Europe and
Central Asia
Latin America
and Caribbean
Middle East /
North Africa
Sub-Saharan
Africa
All developing
countries
2000 75.6 23.8 4.1 7.7 3.5 32.7 147.9
2050
No climate change 52.3 10.1 2.7 5.0 1.1 41.7 113.3
Climate change 59.1 14.5 3.7 6.4 2.1 52.2 138.5
Table 11-2 | Number of undernourished children younger than 5 years of age (in millions) in 2000 and 2050, using the National Center for Atmospheric Research (NCAR)
climate model (and the A2 scenario from AR4). Results assume no effect of heat on farmers’ productivity, and no CO
2
fertilization benefi ts. (Adapted from Nelson et al., 2009).

731
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
a
vailability would drop below levels that applied in the year 2000, and
that child underweight would be approximately 20% higher (in the
absence of carbon enrichment effects). That is, about 25 million children
would be affected (see Table 11-2). Of note, the underweight estimates
do not account for possible improvements in socioeconomic conditions
between 2000 and 2050. However, it was estimated that substantial
improvements would be necessary to counteract the effects of climate
change. These included a 60% increase in yield growth (all crops) over
baseline, 30% faster growth in animal numbers, and a 25% increase in
the rate of expansion of irrigated areas. The second study by Nelson et
al. used a wider range of socioeconomic and climate scenarios but
health impacts were similar to the first study. Estimates of improved
socioeconomic conditions were insufficient to fully offset the potential
impacts of climate change: child underweight was estimated to be
approximately 10% higher with climate change compared to a future
without climate change.
Lloyd et al. (2011) built a model for estimating future stunting driven
by two principal inputs: estimates of undernourishment (i.e., “food-
related” causes of stunting) and socioeconomic conditions (i.e., “non-
food-related” causes of stunting). The former were based on calorie
availability estimates from Nelson et al. (2009), and the latter on GDP
per capita projections and estimates of the Gini index for income
distribution. They estimated that by 2050, under A2 emissions with
moderate to high economic growth and compared to a future without
climate change, there may be a relative increase of severe stunting of
31 to 55% across regions of sub-Saharan Africa and 61% in South Asia.
It should be noted here that severe stunting carries three to four times
the mortality risk of moderate stunting. In a future without climate
change, undernutrition was projected to decline, leading the authors to
conclude that climate change would hold back efforts to reduce child
undernutrition in the most severely affected parts of the world, even
after accounting for the potential benefits of economic growth.
In addition to global studies, regional projections of the impacts of
climate change on undernutrition have also been carried out since AR4.
Grace et al. (2012) modeled the relationship between climate variables
(temperature and precipitation), food production and availability, as
well as child stunting in Kenya. The authors concluded that climate
change will increase the proportion of stunted children in countries
such as Kenya that are dependent on rain-fed agriculture, unless there
are substantial adaptation efforts, such as investment in education and
agricultural technology.
Similarly, Jankowska et al. (2012) included climate, livelihood, and
health variables (stunting and underweight). The authors identified a
link between type of livelihood and risk of undernutrition, and climate
and stunting. Applying the model to Mali, the authors projected impacts
to 2025 and estimated that nearly 6 million people may experience
undernutrition due to changes in climate, livelihood, and demography;
three-quarter to one million of this number will be children younger
than five.
In summary, we conclude that climate change will have a substantial
negative impact on (1) per capita calorie availability; (2) childhood
undernutrition, particularly stunting; and (3) on undernutrition-related
child deaths and DALYs lost in developing countries (high confidence).
11.6.2. Occupational Health
Since AR4, much has been written on the effects of heat on working
people (Kjellstrom et al., 2009a; Dunne et al., 2013) and on other climate-
related occupational health risks (Bennett and McMichael, 2010; Schulte
and Chun, 2009).
11.6.2.1. Heat Strain and Heat Stroke
Worldwide, more than half of all non-household labor-hours occur
outdoors, mainly in agriculture and construction (IFAD, 2010; ILO, 2013).
Individuals who are obliged to work outside in hot conditions, without
access to shade, or sufficient water, are at heightened risk of heat strain
(ICD code T.67, “heat exhaustion”) and heat stroke. Health risks increase
with the level of physical exertion. Agricultural and construction workers
in tropical developing countries are therefore among the most exposed,
but heat stress is also an issue for those working indoors in environments
that are not temperature-controlled, and even for some workers in high-
income countries such as the USA (Luginbuhl et al., 2008; see Figure
11-5). Moreover, at higher temperatures there is potential conflict
between health protection and economic productivity (Kjellstrom et al.,
2011): as workers take longer rests to prevent heat stress, hourly
productivity goes down (Sahu et al., 2013).
11.6.2.2. Heat Exhaustion and Work Capacity Loss
There are international standards of maximum recommended workplace
heat exposure and hourly rest time (e.g., ISO, 1989; Parsons, 2003) for
both acclimatized and non-acclimatized people. In hot countries during
the hot season, large proportions of the workforce are affected by heat,
and the economic impacts of reduced work capacity may be sufficient to
jeopardize livelihoods (Lecocq and Shalizi, 2007; Kjellstrom et al., 2009a,
2011; Kjellstrom and Crowe, 2011). Kjellstrom and Crow (2011) and
Dunne et al. (2013) report that loss of work productivity during the hottest
and wettest seasons has already occurred, at least in Asia and Africa.
11.6.2.3. Other Occupational Health Concerns
In areas where vector-borne diseases, such as malaria and dengue fever,
are common, people working in fields without effective protection may
experience a higher incidence of these diseases when climatic conditions
favor mosquito breeding and biting (Bennett and McMichael, 2010).
Increasing heat exposure in farm fields during the middle of the day may
lead to more work during dawn and dusk when some of the vectors
are biting humans more actively. Exposure to heat affects psychomotor,
perceptual, and cognitive performance (Hancock et al., 2007) and
increases risk of injuries (Ramsey, 1995). Extreme weather events and
climate-sensitive infectious diseases also pose occupational risks to
health workers, which may in turn undermine health protection for the
wider population (WHO, 2009b). Other mechanisms include elevated
occupational exposures to toxic chemical solvents that evaporate faster
at higher temperatures (Bennett and McMichael, 2010) and rising
temperatures reducing sea ice and increasing risk of drowning in those
engaged in traditional hunting and fishing in the Arctic (Ford et al., 2008).
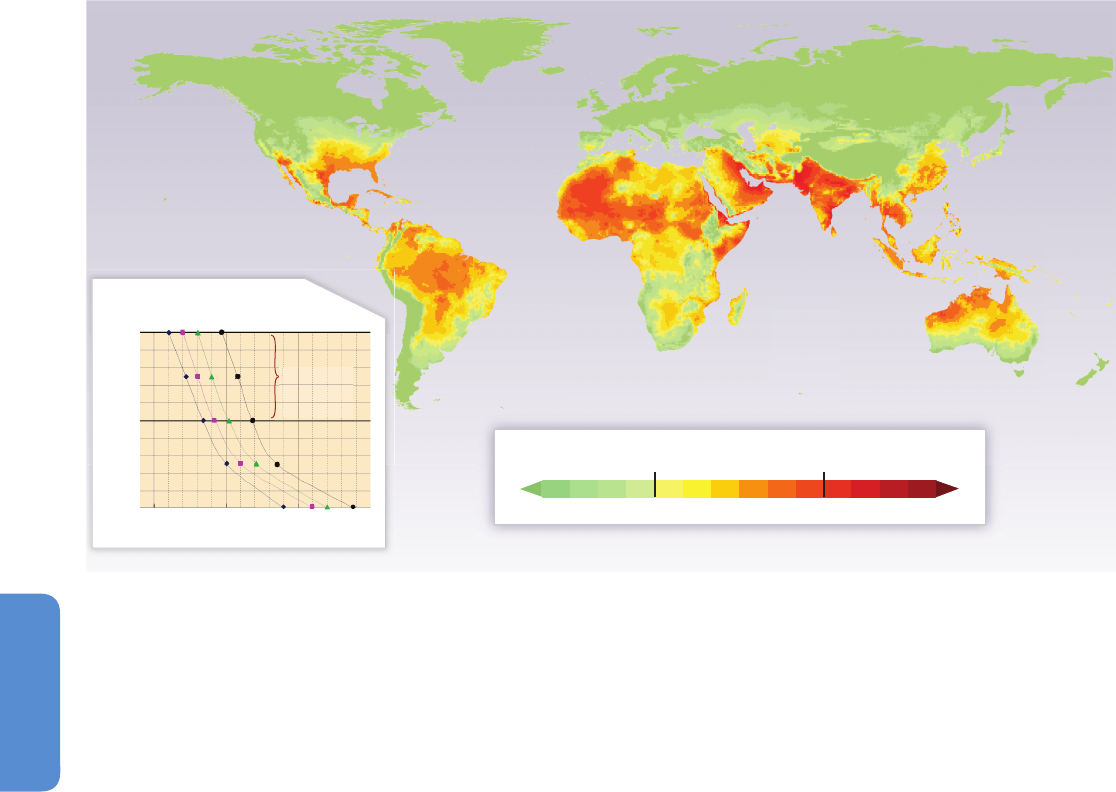
732
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
11.6.2.4. Near-Term Future
Projections have been made of the future effects of heat on work
capacity (Kjellstrom et al., 2009b; Dunne et al., 2013). Temperature and
humidity were both included, and the modeling took into account the
changes in the workforce distribution relating to the need for physical
activity. In Southeast Asia, in 2050, the model indicates that more than
half the afternoon work hours will be lost due to the need for rest
breaks (Kjellstrom et al., 2013). By 2100, under RCP4.5, Dunne et al.
(2013) project up to a 20% loss of productivity globally. There is an
unfortunate trade-off between health impact and productivity, which
creates risks for poor and disenfranchised laborers working under
difficult working conditions and inflexible rules (Kjellstrom et al., 2009a,
2011; Sahu et al., 2013).
11.6.3. Mental Health
Harsher weather conditions such as floods, droughts, and heat waves
tend to increase the stress on all those who are already mentally ill, and
may create sufficient stress for some who are not yet ill to become so
(Berry et al., 2010). Manifestations of disaster-related psychiatric trauma
include severe anxiety reactions (such as post-traumatic stress) and
longer-term impacts such as generalized anxiety, depression, aggression,
and complex psychopathology (Ahern et al., 2005; Ronan et al., 2008).
For slow-developing events such as prolonged droughts, impacts include
chronic psychological distress and increased incidence of suicide (Alston
and Kent, 2008; Hanigan et al., 2012). Extreme weather conditions may
have indirect effects on those with mental illness, through the impacts on
agricultural productivity, fishing, forestry, and other economic activities.
Disasters such as cyclones, heat waves, and major floods may also have
destructive effects in cities. Here again, the mentally ill may be at risk:
cities often feature zones of concentrated disadvantage where mental
disorders are more common (Berry, 2007) and there is also higher risk
of natural disasters (such as flooding).
In addition to effects of extreme weather events on mental health via
the risk/disadvantage cycle, there may be a distressing sense of loss,
known as “solastalgia,” that people experience when their land is
damaged (Albrecht et al., 2007) and they lose amenity and opportunity.
11.6.4. Violence and Conflict
Soil degradation, freshwater scarcity, population pressures, and other
forces that are related to climate are all potential causes of conflict. The
relationships are not straightforward, however, as many factors influence
conflict and violence. The topic is reviewed closely in Chapter 12, which
concludes that factors associated with risk of violent conflict, such as
poverty and impaired state institutions, are sensitive to climate variability,
Low risk Moderate risk High risk
<
20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 >35
H
eat exposure WBGT °C
Figure 11-5 | The 1980–2009 average of the hottest months globally, measured in web bulb globe temperature (WBGT), which combines temperature, humidity, and other
factors into a single index of the impact on work capacity and threat of heat exhaustion. The insert shows the International Organization for Standardization standard (ISO,1989)
for heat stress in the workplace that leads to recommendations for increased rest time per hour to avoid heat exhaustion at different work levels. This is based on studies of
healthy young workers and includes a margin of safety. Note that some parts of the world already exceed the level for safe work activity during the hottest month. In general,
with climate change, for every 1°C that T
max
goes up, the WBGT goes up by about 0.9°C, leading to more parts of the world being restricted for more of the year, with consequent
impacts on productivity, heat exhaustion, and need for air conditioning to protect health (Lemke and Kjellstrom, 2012).
Job exertion required (Watts)
5
0
0
4
0
0
3
0
0
2
0
0
Wet bulb globe temperature (WBGT)
Percent of full working capacity
100
80
6
0
4
0
2
0
0
25˚C 30˚C 35˚C 40˚C
e.g. 2˚C rise
a
pproximately
halves work
output

733
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
b
ut evidence of an effect of climate change on violence is contested.
Also, it is noted that populations affected by violence are particularly
vulnerable to the impacts of climate change on health and social well-
being.
11.7. Adaptation to Protect Health
Climate change may threaten the progress that has been made in
reducing the burden of climate-related disease and injury. The degree
to which programs and measures will need modification to address
additional pressures from climate change will depend on the current
burden of ill health; the effectiveness of current interventions; projections
of where, when, and how the health burden could change with climate
change; the feasibility of implementing additional programs; other
stressors that could increase or decrease resilience; and the social,
economic, and political context for intervention (Ebi et al., 2006).
The scientific literature on adaptation to climate change has expanded
since AR4, and there are many more national adaptation plans that
include health, but investment in specific health protection activities is
growing less rapidly. A review by the World Health Organization in 2012
estimated that commitments to health adaptation internationally
amount to less than 1% of the annual health costs attributable to
climate change in 2030 (WHO Regional Office for Europe, 2013).
The value of adaptation is demonstrated by the health impacts of recent
disasters associated with extreme weather and climate events, although
not necessarily attributed with confidence to climate change itself. For
example, approximately 500,000 people died when Cyclone Bhola
(category 3 in severity) hit East Pakistan (present day Bangladesh) in
1970 (Khan, 2008). In 1991, a cyclone of similar severity caused about
140,000 deaths. In November 2007, Cyclone Sidr (category 4) resulted
in approximately 3400 deaths. The population had grown by more
than 30 million in the intervening period (Mallick et al., 2005).
Bangladesh achieved this remarkable reduction in mortality through
effective collaborations between governmental and non-governmental
organizations and local communities (Khan, 2008).
Alongside improving general disaster education (greatly assisted by
rising literacy rates, especially among women), the country deployed
early warning systems and built a network of cyclone shelters. Early
warning systems included high-technology information systems and
relatively simple measures such as training volunteers to distribute
warning messages by bicycle.
Efforts to adapt to the health impacts of climate change can be
categorized as incremental, transitional, and transformational actions
(O’Brien et al., 2012). Incremental adaptation includes improving
public health and health care services for climate-related health
outcomes, without necessarily considering the possible impacts of
climate change. Transitional adaptation means shifts in attitudes and
perceptions, leading to initiatives such as vulnerability mapping and
improved surveillance systems that specifically integrate environmental
factors. Transformational adaptation (see Chapter 16), which requires
fundamental changes in systems, has yet to be implemented in the
health sector.
11.7.1. Improving Basic Public Health
and Health Care Services
Although the short time period since health adaptation options have
been implemented means evidence of effectiveness in specifically
reducing climate change-related impacts is currently lacking, there is
abundant evidence of steps that may be taken to improve relevant
public health functions (Woodward et al., 2011). This is important
because the present health status of a population may be the single
most important predictor of both the future health impacts of climate
change and the costs of adaptation (Pandey, 2010). Most health
adaptation focuses on improvements in public health functions to
reduce the current adaptation deficit, such as enhancing disease
surveillance, monitoring environmental exposures, improving disaster
risk management, and facilitating coordination between health and
other sectors to deal with shifts in the incidence and geographic range
of diseases (Woodward et al., 2011).
Examples of incremental health care interventions include introduction
of vaccination programs in the USA, after which seasonal outbreaks of
rotavirus, a common climate-sensitive pathogen, were delayed and
diminished in magnitude (Tate et al., 2009). Post-disaster initiatives also
are important. For example, an assessment of actions to improve the
resilience of vulnerable populations to heat waves recommended staff
planning over the summer period, cooling of health care facilities, training
of staff to recognize and treat heat strain, and monitoring of those in the
highest risk population groups (WHO Regional Office for Europe, 2009).
Ensuring essential medical supplies for care of individuals with chronic
conditions, including effective post-disaster distribution, would increase
the ability of communities to manage large-scale floods and storms. In
Benin, one measure proposed as part of the national response to sea
level rise and flooding is expanded health insurance arrangements, so
that diseases such as malaria and enteric infections can be treated
promptly and effectively (Dossou and Glehouenou-Dossou, 2007).
11.7.2. Health Adaptation Policies and Measures
Transitional adaptation moves beyond focusing on reducing the current
adaptation deficit to considerations of how a changing climate could
alter health burdens and the effectiveness of interventions (Frumkin et
al., 2008). For example, maintaining and improving food safety in the
face of rising temperatures and rainfall extremes depends on effective
interactions between human health and veterinary authorities, integrated
monitoring of food-borne and animal diseases, and improved methods
to detect pathogens and contaminants in food (Tirado et al., 2010).
Indicators of community functioning and connectedness also are
relevant because communities with high levels of social capital tend to
be more successful in disseminating health and related messages,
providing support to those in need (Frumkin et al., 2008).
11.7.2.1. Vulnerability Mapping
Vulnerability mapping is being increasingly used to better understand
current and possible future risks related to climate change. For example,
Reid et al. (2009) mapped community determinants of heat vulnerability

734
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
i
n the USA. The four factors explaining most of the variance were a
combination of social and environmental factors, social isolation,
prevalence of air conditioning, and the proportion of the population
who were elderly or diabetic. Remote-sensing technologies are now
sufficiently fine-grained to map local vulnerability. For example, these
technologies can be used to map surface temperatures and urban heat
island effects at the neighborhood scale, indicating where city greening
and other urban cooling measures could be most effective, and alerting
public health authorities to populations that may be at greatest risk of
heat waves (Luber and McGeehin, 2008). In another example, spatial
modeling of geo-referenced climate and environmental information was
used to identify characteristics of domestic malaria transmission in
2009–2012 in Greece, to guide malaria control efforts (Sudre et al.,
2013). Mapping at regional and larger scales may be useful to guide
adaptation actions. In Portugal, modeling of Lyme disease indicates that
future conditions will be less favorable for disease transmission in the
south, but more favorable in the center and northern parts of the
country (Casimiro et al., 2006). This information can be used to modify
surveillance programs before disease outbreaks occur. To capture a
more complete picture of vulnerability, mapping exercises also could
consider climate sensitivity and adaptation capacity, such as was
done in an assessment of climate change and risk of poverty in Africa
(Thornton et al., 2008).
11.7.3. Early Warning Systems
Early warning systems have been developed in many areas to prevent
negative health impacts through alerting public health authorities and
the general public about climate-related health risks. Effective early
warning systems take into consideration the range of factors that can
drive risk and are developed in collaboration with end users.
Components of effective early warning systems include forecasting
weather conditions associated with increased morbidity or mortality,
predicting possible health outcomes, identifying triggers of effective and
timely response plans that target vulnerable populations, communicating
risks and prevention responses, and evaluating and revising the system
to increase effectiveness in a changing climate (Lowe et al., 2011). Heat
wave early warning systems are being increasingly implemented,
primarily in high-income countries. Of seven studies of the effectiveness
of heat wave early warning systems or heat prevention activities to
reduce heat-related mortality, six reported fewer deaths during heat
waves after implementation of the system (Palecki et al., 2001; Weisskopf
et al., 2002; Ebi et al., 2004; Tan et al., 2007; Fouillet et al., 2008; Chau
et al., 2009); only Morabito et al. (2012) was inconclusive. For example,
in the summer of 2006, France experienced high temperatures with
about 2000 excess deaths. This was more than 4000 fewer deaths than
was anticipated on the basis of what occurred in the 2003 heat wave.
A national assessment attributed the lower than expected death toll to
greater public awareness of the health risks of heat, improved health
care facilities, and the introduction in 2004 of a heat wave early warning
system (Fouillet et al., 2008). A review of the heat wave early warning
systems in the 12 European countries with such plans concluded that
evaluations of the effectiveness of these systems is urgently needed to
inform good practices, particularly understanding which actions increase
resilience (Lowe et al., 2011).
E
arly warning systems have been developed also for vector-borne and
food-borne infections, although evidence of their effectiveness in reducing
disease burdens is limited. In Botswana, an early warning system forecasts
malaria incidence up to 4 months in advance based on observed rainfall;
interannual and seasonal variations in climate are associated with
outbreaks of malaria in this part of Africa. Model outputs include
probability distributions of disease risk and measures of the uncertainty
associated with the forecasts (Thomson et al., 2006). A weather-based
forecasting model for dengue, developed in Singapore, predicted
epidemics 13 months ahead of the peak in new cases, which gave the
national control program time to increase control measures (Hii et al.,
2012). A study of campylobacteriosis in the USA developed models of
monthly disease risk with a very good fit in validation data sets (R
2
up
to 80%) (Weisent et al., 2010).
11.7.4. Role of Other Sectors in Health Adaptation
Other sectors—including ecosystems, water supply and sanitation,
agriculture, infrastructure, energy and transportation, land use
management, and others—play an important part in determining the
risks of disease and injury resulting from climate change.
Within the context of the EuroHEAT project, a review of public health
responses to extreme heat in Europe identified transport policies,
building design, and urban land use as important elements of national
and municipal heat wave and health action plans (WHO Regional Office
for Europe, 2009). A study examining well-established interventions
to reduce the urban heat island effect (replacing bitumen and concrete
with more heat-reflective surfaces, and introducing more green spaces
to the city) estimated these would reduce heat-related emergency
calls for medical assistance by almost 50% (Silva et al., 2010). Urban
green spaces lower ambient temperatures, improve air quality, provide
shade, and may be good for mental health (van den Berg et al., 2010).
However, the extent to which changes in these factors reduce heat
wave-related morbidity and mortality depend on location. A study in
London, UK, found that built form and other dwelling characteristics
more strongly influenced indoor temperatures during heat waves
than did the urban health island effect (Oikonomou and Wilkinson,
2012).
A review of food aid programs indicates that a rapid response to the
risk of child undernutrition, targeted to those in greatest need, with
flexible financing and the capacity to rapidly scale up depending on
need, may reduce damaging health consequences (Alderman, 2010).
Community-based programs designed for other purposes can facilitate
adaptation, including disaster risk management. In the Philippines, for
example, interventions in low-income urban settings with the potential
to reduce the harmful effects of climate extremes on health include
savings schemes, small-scale loans, hygiene education, local control and
maintenance of water supplies, and neighborhood level solid waste
management strategies (Dodman et al., 2010). It is important to note
that climate change adaptation in other sectors may influence health
in a positive manner (e.g., re-vegetation of watersheds to improve water
quality), or on occasion, exacerbate health risks (e.g., urban wetlands
designed primarily for flood control may promote mosquito breeding)
(Medlock and Vaux, 2011).
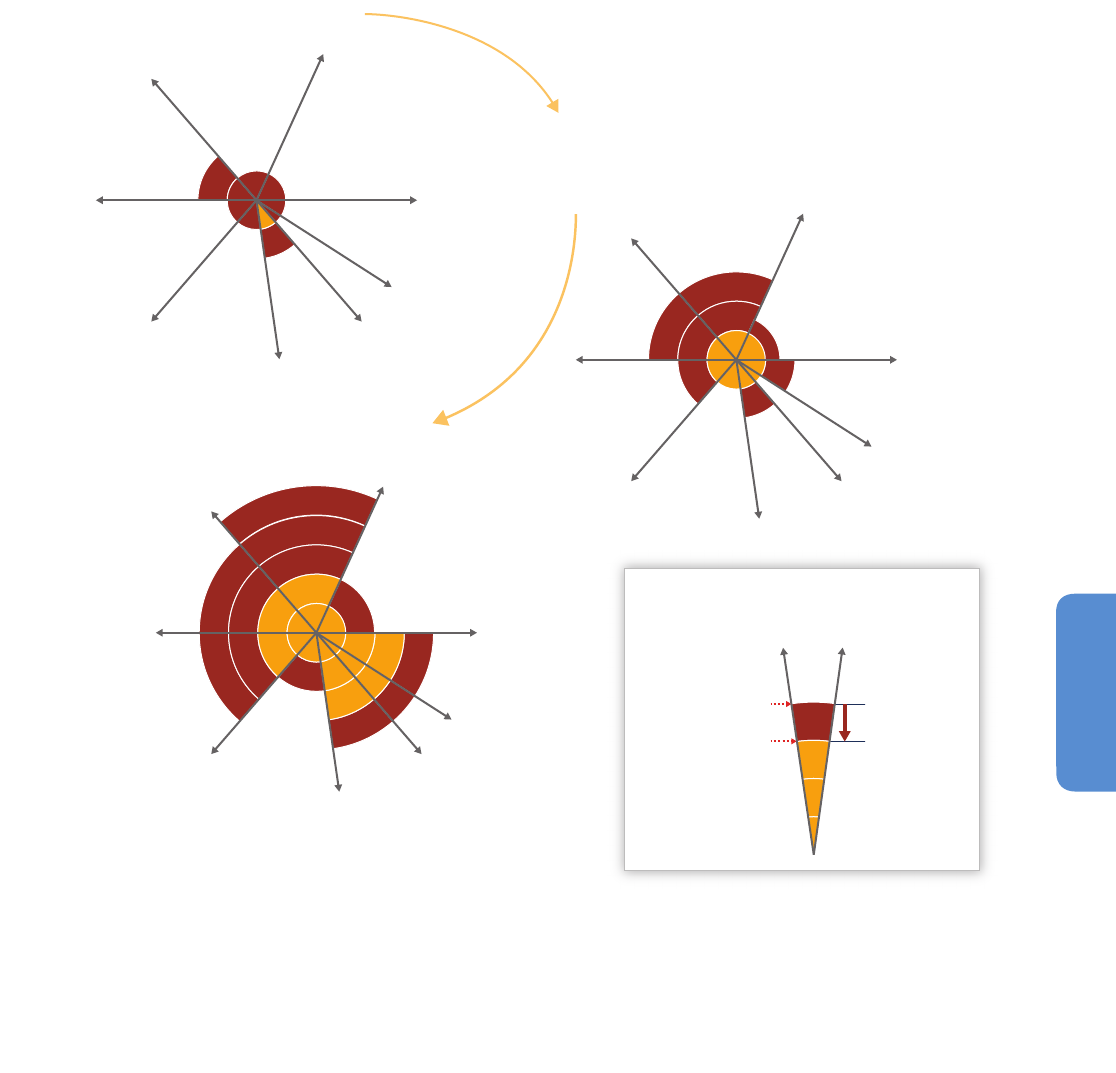
735
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
11.8. Adaptation Limits
Under High Levels of Warming
Most attempts to quantify health burdens associated with future climate
change consider modest increases in global average temperature,
typically less than 2°C. However, research published since AR4 raises
doubt over whether it will be possible to limit global warming to 2°C
above preindustrial temperatures (Rogelj et al., 2009; Anderson and
Bows, 2011; PriceWaterhouseCoopers, 2012). It is therefore increasingly
important to examine the likely health consequences of warming beyond
2°C, including extreme warming of 4°C to 6°C or higher. Predictions of
this nature are limited by uncertainty about climatic as well as key, non-
climatic determinants of health including the nature and degree of
adaptation. Here, we instead focus primarily on physiological or
ecological limits that constrain our ability to adapt and protect human
health and wellbeing (Section 16.4.1).
It can be assumed that the increase in many important climate-related
health impacts at increasingly higher levels of warming will be greater
than simple linear increments; that is, that the health consequences of
a 4°C temperature increase will be more than twice those of a +2°C
world (see Figure 11-6). Nonlinear and threshold effects have been
Potential for
adaptation to
reduce risk
Risk level with
current adaptation
Risk level with
high adaptation
Risk and potential for adaptation
2080–2100
"Era of climate options"
+ 4°C
Present
+ 1.5°C
2030–2040
"Era of committed climate change"
V
ector-borne
d
iseases
Undernutrition
Heat
Food- and
water-borne
infections
Air quality
Extreme
weather
events
Mental health
and violence
Occupational
health
V
ector-borne
d
iseases
Undernutrition
Heat
Food- and
w
ater-borne
i
nfections
Air quality
Extreme
w
eather
e
vents
Mental health
a
nd violence
Occupational
health
Vector-borne
d
iseases
U
ndernutrition
H
eat
F
ood- and
water-borne
infections
A
ir quality
Extreme
w
eather
events
Mental health
a
nd violence
Occupational
health
Figure 11-6 | Conceptual presentation of the health impacts from climate change and the potential for impact reduction through adaptation. Impacts are identified in eight
health-related sectors based on assessment of the literature and expert judgments by authors of Chapter 11. The width of the slices indicates in a qualitative way the relative
importance in terms of burden of ill health globally at present and should not be considered completely independent. Impact levels are presented for the near-term “era of
committed climate change” (2030–2040), in which projected levels of global mean temperature increases do not diverge substantially across emissions scenarios. For some
sectors, for example, vector-borne diseases, heat/cold stress, and agricultural production and undernutrition, there may be benefits to health in some areas, but the net impact is
expected to be negative. Estimated impacts are also presented for the longer-term “era of climate options” (2080–2100), for global mean temperature increase of 4°C above
preindustrial levels, which could potentially be avoided by vigorous mitigation efforts taken soon. For each timeframe, impact levels are estimated for the current state of
adaptation and for a hypothetical highly adapted state, indicated by different colors.

736
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
o
bserved in the mortality response to extreme heat (Anderson and Bell,
2011; McMichael, 2013a), agricultural crop yields, as key determinants
of childhood nutrition and development (Schlenker and Roberts, 2009;
Lobell et al., 2011a), and infectious diseases (Altizer et al., 2006), for
example. These are also briefly elaborated here.
1
1.8.1. Physiological Limits to Human Heat Tolerance
In standard (or typical) conditions, core body temperatures will reach
lethal levels under sustained periods of wet-bulb temperatures above
about 35°C (Sherwood and Huber, 2010). Sherwood and Huber (2010)
conclude that a global mean warming of roughly 7°C above current
temperatures would create small land areas where metabolic heat
dissipation would become impossible. An increase of 11°C to 12°C
would enlarge these zones to encompass most of the areas occupied
by today’s human population. This analysis is likely a conservative
estimate of an absolute limit to human heat tolerance because working
conditions are hazardous at lower thresholds. The U.S. military, for
example, suspends all physical training and strenuous exercise when
the wet-bulb globe temperature (WBGT) exceeds 32°C (Willett and
Sherwood, 2012) while international labor standards suggest the time
acclimatized individuals spend doing low intensity labor such as office
work be halved under such conditions (Kjellstrom et al., 2009a).
1
One
estimate suggests global labor productivity will be reduced during the
hottest months to 60% in 2100 and less than 40% in 2200 under the
RCP8.5 scenario in which global mean temperatures rise 3.4°C by 2100
and 6.2°C by 2200 relative to 1861–1960 (Dunne et al., 2013). It is
projected that tropical and mid-latitude regions including India, Northern
Australia, and the southeastern USA will be particularly badly affected
(Willett and Sherwood, 2012; Dunne et al., 2013).
11.8.2. Limits to Food Production and Human Nutrition
Agricultural crops and livestock similarly have physiological limitations
in terms of thermal and water stress. For example, production of the
staple crops maize, rice, wheat, and soybean is generally assumed to
face an absolute temperature limit in the range of 40°C to 45°C (Teixeira
et al., 2011), while key phenological stages such as sowing to emergence,
grain-filling, and seed set have maximum temperature thresholds near
or below 35°C (Yoshida et al., 1981; Porter and Gawith, 1999; Porter and
Semenov, 2005 ). The existence of critical climatic thresholds and evidence
of nonlinear responses of staple crop yields to temperature and rainfall
(Brázdil et al., 2009; Schlenker and Roberts, 2009; Lobell et al., 2011b)
thus suggest that there may be a threshold of global warming beyond
which current agricultural practices can no longer support large human
civilizations, and the impacts on malnourishment and undernutrition
described in Section 11.6.1 will become much more severe. However,
current models to estimate the human health consequences of climate-
impaired food yields at higher global temperatures generally incorporate
neither critical thresholds nor nonlinear response functions (Lloyd et al.,
2011; Lake et al., 2012), reflecting uncertainties about exposure-response
relations, future extreme events, the scale and feasibility of adaptation,
a
nd climatic thresholds for other influences such as infestations and
plant diseases. Extrapolation from current models nevertheless suggests
that the global risk to food security becomes very severe under an increase
of 4°C to 6°C or higher in global mean temperature (medium evidence,
high agreement) (Chapter 7, Executive Summary).
1
1.8.3. Thermal Tolerance of Disease Vectors
Substantial warming in higher-latitude regions will open up new
terrain for some infectious diseases that are limited at present by low
temperature boundaries, as already evidenced by the northward
extensions in Canada and Scandinavia of tick populations, the vectors
for Lyme disease and tick-borne encephalitis (Lindgren and Gustafson,
2001; Ogden et al., 2006). On the other hand, the emergence of new
temperature regimes that exceed optimal conditions for vector and host
species will reduce the potential for infectious disease transmission and,
with high enough temperature rise, may eventually eliminate some
infectious diseases that exist at present close to their upper tolerable
temperature limits. For example, adults of two malaria-transmitting
mosquito species are unable to survive temperatures much above 40°C
in laboratory experiments (Lyons et al., 2012), although in the external
world they may seek out tolerable microclimates. Reproduction of the
malaria parasite within the mosquito is impaired at lesser raised
temperatures (Paaijmans et al., 2009). Larval development of Aedes
albopictus, an Asian mosquito vector of dengue and chikungunya, also
does not occur at or above 40°C (Delatte et al., 2009).
11.8.4. Displacement and Migration
Under Extreme Warming
Weather extremes and longer term environmental change including sea
level rise lead to both more people displaced and increase in populations
that are effectively trapped (Section 12.4.1.2). This trend is expected to
be more pronounced under extreme levels of warming (Section 16.5).
Gemenne (2011) argues that the most significant difference between
the nature of human migration in response to 4°C of warming relative
to 2°C would be to remove many people’s ability to choose whether to
stay or leave when confronted with environmental changes. Health
studies of refugees, migrants, and people in resettlement schemes suggest
that forced displacement, in turn, is likely to lead to more adverse health
impacts than voluntary migration or planned resettlement (McMichael
et al., 2012). The health risks associated with forced displacement include
undernutrition; food- and water-borne illnesses; diseases related to
overcrowding such as measles, meningitis, and acute respiratory
infections; sexually transmitted diseases; increased maternal mortality;
and mental health disorders (McMichael et al., 2012).
11.8.5. Reliance on Infrastructure
Under severe climate regimes, societies may be able to protect themselves
by enclosing places for living and working, first for their most vulnerable
1
WBGT is a heat index closely related to the wet-bulb temperature that also incorporates measures of radiant heat from the sun and evaporative cooling due to wind.
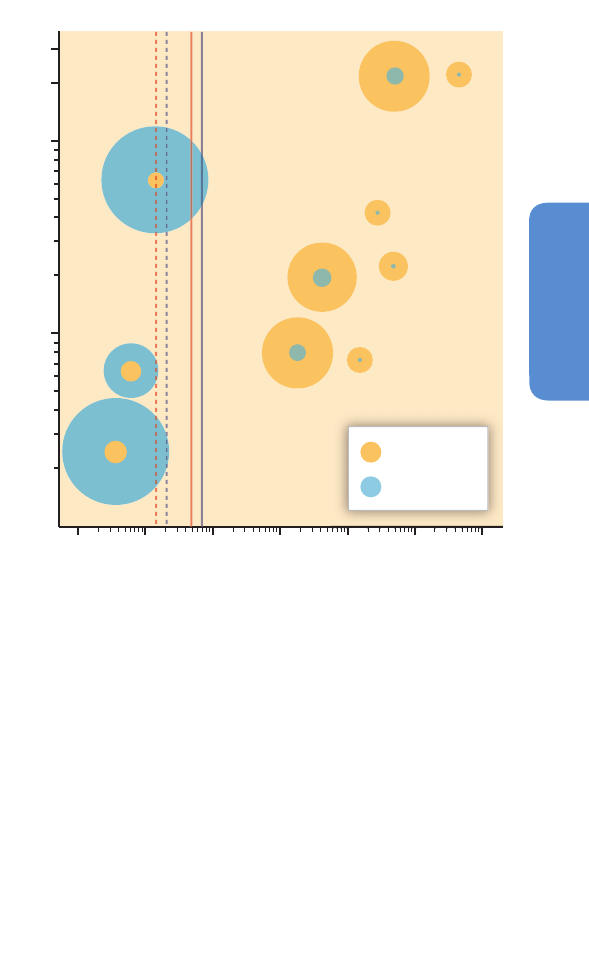
737
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
m
embers: the young, old, ill, and manual laborers. This strategy will
mean increased vulnerability to infrastructure failure and unreliable
energy and water supplies. Electrical power outages have been linked
to both accidental and disease-related deaths in temperate climates
(Anderson and Bell, 2012), and failures in power supplies are more likely
to occur during extreme weather events (Section 19.6.2.1). Large-scale
reliance on air conditioning under a significantly hotter climate regime
would therefore pose a serious health risk.
11.9. Co-Benefits
Essentially every human activity affects (and is affected by) climate and
health status in some way, but not all are strongly linked to either and
even fewer strongly to both. Here we focus on measures to mitigate
the atmospheric concentration of warming climate-altering pollutants
that also hold the potential to significantly benefit human health. These
so-called co-benefits include health gains from strategies that are directed
primarily at climate change, and mitigation of climate change from well-
chosen policies for health advancement (Haines et al., 2007; Apsimon
et al., 2009; Smith and Balakrishnan, 2009; UNEP, 2011; Shindell et al.,
2012). The literature on health co-benefits associated with climate
change mitigation strategies falls into several categories (Smith and
Balakrishnan, 2009; Smith et al., 2009). These include:
• Reduce emissions of health-damaging pollutants, either primary or
precursors to other pollutants in association with changes in energy
production, energy efficiency, or control of landfills
• Increase access to reproductive health services
• Decrease meat consumption (especially from ruminants) and
substitute low-carbon healthy alternatives
• Increase active transport particularly in urban areas
• Increase urban green space.
In addition, although not discussed here, there are potential health
side effects of mitigation measures, such as geoengineering, biofuel
expansion, and carbon taxes that are potentially deleterious for human
health (Tilman et al., 2009; see Chapter 19). In Table 11-3, we summarize
what is known about the main categories of co-benefits, but because
of space limitation, we only provide additional detail for two of them
below.
11.9.1. Reduction of Co-Pollutants
Most of the publications related to CAPs and health-damaging
pollutants refer to fuel combustion and fall into three major categories:
(1) improvement in energy efficiency will reduce emissions of CO
2
and
health-damaging pollutants, providing these gains are not outpaced by
increases in energy demand, and the energy is derived from combustion
of fossil fuels or non-renewable biomass fuels, either directly or
through the electric power system; (2) increases of combustion efficiency
(decreasing emission of incomplete combustion products) will have
both climate and health benefits, even if there is no change in energy
efficiency and/or fuel itself is renewable, because a number of the
products of incomplete combustion are climate altering and nearly all are
damaging to health (Smith and Balakrishnan, 2009); and (3) increased
use of non-combustion sources, such as wind, solar, tidal, wave, and
g
eothermal energy, would reduce emissions of warming CAPs and
health damaging air pollutants, providing benefits for climate and
health (Jacobson et al., 2013).
Studies of the health co-benefits of reduction in air pollutants include
sources that produce outdoor air pollution (Bell et al., 2008a) and
household sources (Po et al., 2011). In many parts of the world,
household fuels (poorly combusted biomass and coal) are responsible
for a substantial percent of primary outdoor fine particle pollution as
well, perhaps a quarter in India for example (Lim et al., 2012). In many
parts of the world, household fuel (poorly combusted biomass and coal)
is responsible for much fine particle outdoor air pollution and may
contribute to long-range transport of hazardous air pollutants (Anenberg
et al., 2013). This indicates that reductions in emissions from household
sources will yield co-benefits through the outdoor pollution pathway.
Figure 11-7 | Illustrative co-benefits comparison of the health and climate
cost-effectiveness of selected household, transport, and power sector interventions
(Smith and Haigler, 2008). Area of each circle denotes the total social benefit in
international dollars (Int$) from the combined value of carbon offsets (valued at
10$/tCO
2
-eq (tons of carbon dioxide equivalent)) and averted disability-adjusted life
years (DALYs; $7450/DALY, which is representative of valuing each DALY at the
average world gross domestic product (PPP) per capita in 2000). The vertical lines
shows the range of the cut offs for cost-effective (solid lines) and very cost-effective
(dashed lines) health interventions in India (red lines) and China (purple lines) using
the WHO CHOICE (CHOosing Interventions that are Cost-Effective) criteria (WHO,
2003). This figure evaluates only a small subset of all co-benefits opportunities, and
thus should not be considered either current or complete. It does illustrate, however,
the kind of comparisons that can help distinguish and prioritize options. Note that
even with the log-log scaling, there are big differences among them. For other figures
comparing the climate and health benefits of co-benefits actions including those in
food supply and urban design, see Haines et al. (2009). See the original reference for
details of the calculations in this figure (Smith and Haigler, 2008).
tCO
2
-eq offset
DALYs avoided
Carbon cost effectiveness ($Int/tCO
2
-eq)
United States:
hybrid vehicles
United States:
n
uclear
United States: wind
C
hina: wind
China:
solar PV
United States:
s
olar PV
China: nuclear
China: household
coal to biomass
gasifier stoves
India: improved
biomass stoves
China:
household coal to
p
ropane/LPG stoves
300
100
10
1
1
00,0
00,
000
10
,0
00,
000
1,
000
,000
100
,000
10
,00
0
1
,00
0
1
00
Health cost effectiveness (Int$/DALY)
738
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
If interventions result in reductions in coal combustion, there are a range
of other potential health benefits beyond reduction of particulate air
pollution emissions, including reducing other types of health-damaging
emissions and the human impacts from coal mining (Lockwood, 2012;
Smith et al., 2013).
Another category of air pollution co-benefits comes from controls on
methane emissions that both reduce radiative forcing and potentially
reduce human exposures to ambient ozone, for which methane is a
precursor.
11.9.1.1. Outdoor Sources
Primary co-pollutants, such as particulate matter (PM) and carbon
monoxide (CO) are those released at the point of combustion, while
secondary co-pollutants, such as tropospheric ozone and sulfate particles,
are formed downwind from the combustion source via atmospheric
chemical interactions (Jerrett et al., 2009) and can be transported long
distances.
The burden of disease from outdoor exposures in a country may often be
greater in populations with low socioeconomic status, both because of
living in areas with higher exposures and because these populations often
have worse health and are subjected to multiple additional negative
environmental and social exposures (Morello-Frosch et al., 2011).
11.9.1.2. Household Sources
Globally, the largest exposures from the pollutants from poor fuel
combustion occur in the poorest populations. This is because household
use of biomass for cooking is distributed nearly inversely with income.
Essentially, no poor family can afford gas or electricity for cooking and
very few families who can afford to do so, do not. Thus, the approximate
41% of all world households using solid fuels for cooking are all among
Co-benefi t category Benefi ts for health Benefi ts for climate References
Reduction of co-pollutants from household
s
olid fuel combustion (see also WGIII AR5,
Chapters 7 to 10)
Potentially reduce exposures that are associated
w
ith disease, chronic and acute respiratory
illnesses, lung cancer, low birth weight and
s
tillbirths, and possibly tuberculosis
Reduces CAP emissions associated
w
ith household solid fuel use
including CO
2
, CO, black carbon,
a
nd CH
4
Bell et al. (2008); Smith et al. (2008);
W
ilkinson et al. (2009); Lefohn et al. (2010);
Venkataraman et al. (2010); World Health
O
rganization Regional Offi ce for Europe
(
2010); Po et al. (2011); Anenberg et al. (2012)
Reduction of greenhouse gases and
a
ssociated co-pollutants from industrial
s
ources, such as power plants and landfi lls, by
more effi cient generation or substitution of
l
ow carbon alternatives (Section 27.3.7.2)
Reductions in health-damaging co-pollutant
e
missions would decrease exposures to outdoor air
p
ollution and could reduce risks of cardiovascular
disease, chronic and acute respiratory illnesses,
l
ung cancer, and preterm birth.
Reductions in emissions of CO
2
, black
c
arbon, CO, CH
4
,
and other CAPs
Bell et al. (2008); Apsimon et al. (2009);
J
acobson (2009); Puppim de Oliveira et al.
(
2009); Smith et al. (2009); Tollefsen et al.
(2009); Dennekamp et al. (2010); Jacobson
(
2010); Nemet et al. (2010); Rive and Aunan
(2010); Shonkoff et al. (2011); Shindell et al.
(
2012); West et al. (2012); West et al. (2013)
Energy effi ciency. Actual energy reduction
may sometimes be less than anticipated
b
ecause part of the effi ciency benefi t is taken
as more service.
Reductions in fuel demand potentially can reduce
emissions of CAPs associated with fuel combustion
a
nd subsequent exposures to pollutants that are
known to be health damaging.
Reductions in emission of CAPs due
to decreases in fuel consumption
Markandya et al. (2009); Wilkinson et al. (2009)
I
ncreases in active travel and reductions in
pollution due to modifi cations to the built
e
nvironment, including better access to
public transport and higher density of urban
settlements (see also Sections 24.4, 24.5,
2
4.6, 24.7, 26.8)
I
ncreased physical activity; reduced obesity;
reduced non-communicable disease burden, health
s
ervice costs averted; improved mental health;
reduced exposure to air pollution; increased local
access to essential services, including food stores;
e
nhanced safety
R
eductions of CAP emissions
associated with vehicle transport;
r
eplacing existing vehicles with lower
emission vehicles could reduce air
pollution.
B
abey et al. (2007); Reed and Ainsworth
(2007); Kaczynski and Henderson (2008);
C
asagrande et al. (2009); Jarrett et al. (2009);
Rundle et al. (2009); Woodcock et al. (2009);
Durand et al. (2011); Grabow et al. (2011);
M
cCormack and Shiell (2011); Jensen et al.
(2013); Woodcock et al. (2013)
H
ealthy low greenhouse gas emission diets,
which can have benefi cial effects on a range
o
f health outcomes (see also Table 11.3)
R
educed dietary saturated fat in some populations
(particularly from ruminants) and replacement by
p
lant sources associated with decreased risk of
(ischemic) heart disease, stroke, colorectal cancer
(processed meat consumption). Increased fruit
and vegetable consumption can reduce risk of
chronic diseases. Reduced CH
4
emissions due to
a decreased demand for ruminant meat products
would reduce tropospheric ozone.
R
eductions in CO
2
and CH
4
emissions
from energy-intensive livestock
s
ystems
M
cMichael et al. (2007); Friel et al. (2009);
Sinha et al. (2009); Smith and Balakrishnan
(
2009); Jakszyn et al. (2011); Hooper et al.
(2012); Pan et al. (2012); Xu et al. (2012)
Greater access to reproductive health services Lower child and maternal mortality from increased
birth intervals and shifts in maternal age
Potentially slower growth of energy
consumption and related CAP
emissions; less impact on land use
change, etc.
Tsui et al. (2007); Gribble et al. (2009); Prata
(2009); O’Neill et al. (2010); Diamond-Smith
and Potts (2011); Potts and Henderson (2012);
Kozuki et al. (2013)
Increases in urban green space (Table 25-5) Reduced temperatures and heat island effects;
reduced noise; enhanced safety; psychological
benefi ts; better self-perceived health status
Reduces atmospheric CO
2
via carbon
sequestration in plant tissue and soil
Mitchell and Popham (2007); Babey et al.
(2008); Maas et al. (2009); van den Berg et al.
(2010); van Dillen et al. (2011)
Carbon sequestration in forest plantations,
reducing emissions from deforestation and
degradation, and carbon offset sales (see
Chapter 13 and Section 15.3.4; see also
Sections 20.4.1 and 26.8.4.3)
Poverty alleviation and livelihood / job generation
through sale of Clean Development Mechanism
and voluntary market credits. Ameliorate
declines in production or competitiveness in rural
communities
Reduces emissions of CAPs and
promotes carbon sequestration
through reducing emissions from
deforestation and degradation
Holmes (2010); Ezzine-de-Blas et al. (2011)
Table 11-3 | Examples of recent (post-AR4) research studies on co-benefi ts of climate change mitigation and public health policies. For recent estimates of the global and
regional burden of disease from the various risk factors involved, see Lim et al. (2012). (CAP = climate-altering pollutant.)

739
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
t
he poor in developing countries (Bonjour et al., 2013). Although
biomass makes up the bulk of this fuel and creates substantial health
impacts from products of incomplete combustion when burned in simple
stoves (Lim et al., 2012), probably the greatest health and largest
climate impacts per household result from use of coal, which can also
be contaminated with sulfur and a range of toxic elements as well
(Edwards et al., 2004; Zhang and Smith, 2007). Successfully accelerating
the reduction of impacts from these fuels, however, has not been found
to be easily accomplished with biomass/coal stove programs implemented
to date and may require moving to clean fuels (Bruce et al., 2013). The
climate benefits from improving household biomass fuel combustion
come in part from potential reduction of net warming by reducing
emissions of aerosols (including black carbon), but more confidently
from reduction of CH
4
and other CAPs that are produced by incomplete
combustion, as well as reductions in net CO
2
emissions if interventions
are applied in areas relying on non-renewably harvested wood fuel
(WGI AR5 Section 8.5.3).
11.9.1.3. Primary Co-Pollutants
Outdoor exposure to PM, especially to particles with diameters less than
2.5 µm (PM
2.5
), contributes significantly to ill health including cardio-
and cerebrovascular disease, adult chronic and child acute respiratory
illnesses, lung cancer, and possibly other diseases. The Comparative Risk
Assessment (CRA) for outdoor air pollution done as part of the Global
Burden of Disease (GBD) 2010 Project found approximately 3.2 million
premature deaths globally from ambient particle pollution or about 3%
of the global burden of disease (Lim et al., 2012). Importantly, reductions
in ambient PM concentrations have also been shown to decrease
morbidity and premature mortality (Boldo et al., 2010). A significant
portion of ambient particle pollution derives from fuel combustion,
perhaps 80% globally (GEA, 2012).
Because of higher exposures, an additional set of diseases has also been
associated with combustion products in households burning biomass
and/or coal for cooking and heating. Thus, in addition to the diseases noted
above, cataracts, low birth weight, and stillbirth have been associated
strongly with exposures to incomplete combustion products, such as PM
and CO. CO has impacts on unborn children in utero through exposures
to their pregnant mothers (WHO Regional Office for Europe, 2010).
There is also growing evidence of exacerbation of tuberculosis (Pokhrel
et al., 2010) in adults and cognitive effects in children (Dix-Cooper et al.,
2012). The CRA of the GBD-2010 found 3.5 million premature deaths
annually from household air pollution derived from cooking fuels or
4.4% of the global burden of disease (Lim et al., 2012). Importantly,
there are also studies showing health benefits of household interventions,
for child pneumonia (Smith et al., 2011), blood pressure (McCracken et
al., 2007; Baumgartner et al., 2011) , lung cancer (Lan et al., 2002), and
chronic obstructive pulmonary disease (Chapman et al., 2005). Another
half a million premature deaths are attributed to household cookfuel’s
contribution to outdoor air pollution, making a total of about 4 million
in 2010 or 4.9% of the global burden of disease (Lim et al., 2012).
Black carbon (BC), a primary product of incomplete combustion, is both
a strong CAP and health-damaging (IPCC, 2007; Ramanathan and
Carmichael, 2008; Bond et al., 2013). A systematic review, meta-analysis,
a
nd the largest cohort study to date of the health effects of BC found
that there were probably stronger effects on mortality from exposure
to BC than for undifferentiated fine particles (PM
2.5
) (Smith et al., 2009).
Reviews have concluded that abatement of particle emissions including
BC represents an opportunity to achieve both climate mitigation and
health benefits (UNEP, 2011; Shindell et al., 2012). WGI AR5 (Box TS-6),
however, concluded that the net impact of BC emissions reductions
overall is not certain as to sign, i.e., whether net warming or cooling.
Nevertheless, there would be co-benefits in circumstances where BC is
emitted without many other cooling aerosols, as with diesel and
kerosene combustion (Lam et al., 2012).
Other examples of climate forcing, health-damaging co-pollutants of
CO
2
from fuel use are carbon monoxide, non-methane hydrocarbons,
and sulfur and nitrogen oxides. Each co-pollutant poses risks as well as
being climate altering in different ways. See WGI for more on climate
potential and WHO reviews of health impacts (WHO, 2006; WHO
Regional Office for Europe, 2010).
11.9.1.4. Secondary Co-Pollutants
In addition to being a strong GHG, methane is also a significant
precursor to regional anthropogenic tropospheric ozone production, which
itself is both a GHG and damaging to health, crops, and ecosystems
(WGI AR5 TS.5.4.8). Thus, reductions in CH
4
could lead to reductions in
ambient tropospheric ozone concentrations, which in turn could result
in reductions in population morbidity and premature mortality and climate
forcing.
One study found that a reduction of global anthropogenic CH
4
emissions
by 20% beginning in 2010 could decrease the average daily maximum
8-hour surface ozone by 1 ppb by volume, globally—sufficient to prevent
30,000 premature all-cause mortalities globally in 2030, and 370,000
between 2010 and 2030 (West et al., 2012). CH
4
emissions are generally
accepted as the primary anthropogenic source of tropospheric ozone
concentrations above other human-caused emissions of ozone precursors
(West et al., 2007b), and thus the indirect health co-benefits of CH
4
reductions are epidemiologically significant. On the other hand, work
done for the GBD-2010 estimated 150,000 premature deaths from all
ozone exposures globally in 2010, indicating a more conservative
interpretation of the evidence for mortality from ozone (Lim et al., 2012).
In an analysis of ozone trends from 1998–2008 in the USA, Lefohn et
al. (2010) found that 1-hour and 8-hour ambient ozone averages have
either decreased or failed to increase due to successful regulations of
ozone precursors, predominantly NO
x
and CH
4
. This is consistent with
the EPA (2013) conclusion that in the USA, for the period 1980–2012,
emissions of nitrogen oxides and volatile organic compounds fell by
59% and 57%, respectively (Lefohn et al., 2010; EPA, 2013). These results
point to the effectiveness of reducing ambient ozone concentrations
through regulatory tools that reduce the emissions of ozone precursors,
some of which, like CH
4
, are GHGs.
Not every CAP emitted from fuel combustion is warming. The most
prominent example is sulfur dioxide emitted from fossil fuel combustion,
which changes to particle sulfate in the atmosphere. Although health

740
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
d
amaging, sulfate particles have a cooling effect on global radiative
forcing. Thus, reduction of sulfur emissions, which is important for health
protection, does not qualify as a co-benefit activity because it actually
acts to unmask more of the warming effect of other CAP emissions
(Smith et al., 2009).
1
1.9.1.5. Case Studies of Co-Benefits of Air Pollution Reductions
A recent United Nations Environment Programme (UNEP)- and World
Meteorological Organization (WMO)-led study of BC and tropospheric
ozone found that, if all of 400 proposed BC and CH
4
mitigation measures
were implemented on a global scale, the estimated benefits to health
would come predominately from reducing PM
2
.5
(0.7 to 4.6 million
avoided premature deaths; 5.3 to 37.4 million avoided years of life lost)
compared to tropospheric ozone (0.04 to 0.52 million avoided premature
deaths; 0.35 to 4.7 million avoided years of life lost) based on 2030
population figures (UNEP, 2011). About 98% of the avoided deaths
would come from reducing PM
2.5
, with 80% of the estimated health
benefits occurring in Asia (Anenberg et al., 2012). Another study of the
reduction of PM and ozone exposures due to CAPs emissions controls
and including climate change feedback showed potential reductions of
1.3 million premature deaths by 2050 with avoided costs of premature
mortality many times those of the estimated cost of abatement (West
et al., 2013).
A study of the benefits of a hypothetical 10-year program to introduce
advanced combustion cookstoves in India found that in addition to
reducing premature mortality by about 2 million and DALYs by 55 million
over that period, there would be a reduction of 0.5 to 1.0 billion tons
CO2-eq (Wilkinson et al., 2009). Another study of India found a potential
to reduce 570,000 premature deaths a year, one-third of national BC
emissions, and 4% of all national GHG emissions by hypothetical
substitution of clean household fuel technologies (Venkataraman et al.,
2010).
In their estimation of effects of hypothetical physical and behavioral
modifications in UK housing, Wilkinson and colleagues (Wilkinson et
al., 2009) found that the magnitude and direction of implications for
health depended heavily on the details of the intervention. However,
the interventions were found to be generally positive for health. In a
strategy of housing modification that included insulation, ventilation
control, and fuel switching, along with behavioral changes, it was
estimated that 850 fewer DALYs, and a savings of 0.6 megatonnes of CO
2
per million population in 1 year, could be achieved. These calculations
were made by comparing the health of the 2010 population with and
without the specified physical and behavioral modifications (Wilkinson
et al., 2009).
Markandya et al. (2009) assessed the changes in emissions of PM
2.5
and
subsequent effects on population health that could result from climate
change mitigation measures aimed to reduce GHG emissions by 50%
by 2050 (compared with 1990 emissions) from the electricity generation
sector in the EU, China, and India. In all three regions, changes in modes
of production of electricity to reduce CO
2
emissions were found to reduce
PM
2.5
and associated mortality. The greatest effect was found in India
and the smallest in the EU. The analysis also found that if the health
b
enefits were valued similarly to the approach used by the EU for air
pollution, they offset the cost of GHG emission reductions, especially in
the Indian context where emissions are high but costs of implementing
the measures are low (Markandya et al., 2009).
11.9.2. Access to Reproductive Health Services
Population growth influences the consumption of resources and emissions
of CAPs (Cohen, 2010). Although population growth rates and total
population size do not alone determine emissions, population size is an
important factor. One study showed that CO
2
emissions could be lower
by 30% by 2100 if access to contraception was provided to those
women expressing a need for it (O’Neill et al., 2012). Providing the
unmet need for these services in areas such as the Sahel region of Africa
that has both high fertility and high vulnerability to climate change
can potentially significantly reduce human suffering as climate change
proceeds (Potts and Henderson, 2012).
This is important not only in poor countries, however, but also some rich
ones like the USA, where there is unmet need for reproductive health
services as well as high CO
2
emissions per capita (Cohen, 2010). Also,
because of income rise in developing countries and concurrent reduction
of greenhouse emissions in developed countries, a convergence in
emissions per capita is expected in most scenarios by 2100 (WGI AR5
TS.5.2). Slowing population growth through lowering fertility, as
might be achieved by increasing access to family planning, has been
associated with improved maternal and child health—the co-benefit—
in two main ways: increased birth spacing and reducing births by very
young and old mothers.
11.9.2.1. Birth and Pregnancy Intervals
Current evidence supports, with medium confidence, that short birth
intervals (defined as birth intervals ≤24 months and inter-pregnancy
intervals <6 months) are associated with increased risks of uterine
rupture and bleeding (placental abruption and placenta previa) (Bujold
et al., 2002; Conde-Agudelo et al., 2007).
There is also a correlation between short birth interval and elevated risk
of low birth weight (Zhu, 2005). Zhu (2005) found, in a review of three
studies performed in the USA, that the smallest risk of low birth weight
was found with inter-pregnancy spacing between 18 and 23 months.
Another review of five cohort studies found that a birth interval shorter
than 18 months was significantly associated with increased low
birth weight, preterm birth, and infant mortality after controlling for
confounding factors (Kozuki et al., 2013).
Although an ecological analysis, a review across 17 countries shows a
strikingly coherent picture of the relationship between birth spacing
and reductions in child, infant, and neonatal mortality, with risk of child
undernutrition and mortality both increasing with shorter birth intervals
(Rutstein, 2005). One study estimated that shifting birth spacing from
current patterns in the world to a minimum of 24 months would reduce
by 20% (approximately 2 million) the current excess child mortality in
the world (Rutstein, 2005; Gribble et al., 2009).

741
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
11.9.2.2. Maternal Age at Birth
Risk of death during delivery is highest in very young and very old
mothers, and these are also the age groups that most often want to
control their fertility (Engelman, 2010). Women who begin child bearing
under the age of 20 years are at an increased risk of developing pregnancy
complications such as cephalopelvic disproportion, obstructed labor,
preterm delivery, toxemia, bleeding, and maternal death (Tsui et al.,
2007). In addition, children born to women younger than the age of 20
are at increased risk of fetal growth retardation and low birth weight,
both of which can lead to long-term physical and mental developmental
problems (Tsui et al., 2007). Childbearing at later ages (>35 years) is
associated with increased risk of miscarriage and other adverse health
outcomes (Cleary-Goldman et al., 2005; Ujah et al., 2005).
Providing access to family planning saves women’s lives by reducing
the total number of births and, in particular, through the reduction of
births in high-risk groups (Prata, 2009) while simultaneously reducing
total fertility and subsequent CAP emissions. Studies have found that
when women have access to family planning, it is the highest risk age
groups (youngest and oldest women) who reduce their fertility the most.
In other words, family planning has a differential impact on maternal
mortality reduction through reducing births in the highest risk groups
(Diamond-Smith and Potts, 2011).
11.10. Key Uncertainties and Knowledge Gaps
There is evidence that poverty alleviation, public health interventions
such as provision of water and sanitation, and early warning and response
systems for disasters and epidemics will help to protect health from climate
risks. The key uncertainty is the extent to which society will strengthen
these services, including taking into account the risks posed by climate
change. With a strong response, climate change health effects are
expected to be relatively small in the next few decades, but otherwise
climate-attributable cases of disease and injury will steadily increase.
Since AR4, national governments, through the World Health Assembly,
have specifically called for increased research on (1) the scale and nature
of health risks from climate change; (2) effectiveness of interventions
t
o protect health; (3) health implications of adaptation and mitigation
decisions taken in other sectors, (4) improvement in decision support
systems and surveillance, and (5) estimation of resource requirements.
A recent scoping review identified quantitative peer-reviewed studies
across all of these areas, with the exception of studies on the effectiveness
or cost-effectiveness of targeted adaptation measures (Hosking and
Campbell-Lendrum, 2012). There are also comparatively few studies of
vulnerability in low- and middle-income populations, or of more complex
disease pathways, such as the effect of more extreme weather on water
and sanitation provision and diarrhea rates, on zoonotic diseases, or
mental health. Studies of health co-benefits of climate change mitigation
policies also remain rare compared to the size of the potential health
gains. Potential negative side effects also need to be addressed, for
example those arising from biofuel policies that compete with food
production.
Relevant research for health protection in the near term is therefore
likely to come from cross-disciplinary studies, including public health
decision makers, in the following areas: improved vulnerability and
adaptation assessments that focus on particularly vulnerable populations
and encompass complex causal pathways; quantitative estimation of the
effectiveness of health adaptation measures; surveillance, monitoring,
and observational systems that link climate, health, and economic
impact data and provide a basis for early warning systems as well as
development of future scenarios; and assessment of the health co-
benefits of alternative climate mitigation policies.
In the longer term, research will need to make the best use of traditional
epidemiologic methods, while also taking into account the specific
characteristics of climate change. These include the long-term and
uncertain nature of the exposure and effects on multiple physical and
biotic systems, with the potential for diverse and widespread effects,
including high-impact events. There are low-probability, but plausible,
scenarios for extreme climate regimes before the end of the century.
Although difficult, it is important to develop robust methods to
investigate the health implications of conditions that may apply in 2100,
as decisions today about mitigation will determine their likelihood.
Given the increase globally in life expectancies, many babies born this
decade will be alive at the end of the century, and will be personally
affected by the climate that is in place in 2100.
Frequently Asked Questions
FAQ 11.1 | How does climate change affect human health?
Climate change affects health in three ways: (1) directly, such as the mortality and morbidity (including “heat
exhaustion”) due to extreme heat events, floods, and other extreme weather events in which climate change may
play a role; (2) indirect impacts from environmental and ecosystem changes, such as shifts in patterns of disease-
carrying mosquitoes and ticks, or increases in waterborne diseases due to warmer conditions and increased
precipitation and runoff; and (3) indirect impacts mediated through societal systems, such as undernutrition and
mental illness from altered agricultural production and food insecurity, stress, and violent conflict caused by
population displacement; economic losses due to widespread “heat exhaustion” impacts on the workforce; or other
environmental stressors, and damage to health care systems by extreme weather events.
742
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Fr
e
que
nt
l
y
As
k
e
d
Q
ue
s
t
i
ons
FAQ 11.2 | Will climate change have benefits for health?
Y
e
s
.
F
or
e
x
a
m
ple
s
om
e
popul
a
t
i
ons
in t
e
m
pe
r
a
t
e
a
r
e
a
s
m
a
y
be
a
t
le
s
s
r
i
s
k
f
r
om
e
x
t
r
e
m
e
cold,
a
nd m
a
y
be
ne
fi
t
f
r
om
gr
e
a
t
e
r
a
gr
i
cul
t
ur
a
l
pr
oduct
i
v
i
t
y
,
a
t
l
e
a
s
t
f
or
m
ode
r
a
t
e
de
gr
e
e
s
of
cl
i
m
a
t
e
cha
nge
.
S
om
e
a
r
e
a
s
cur
r
e
nt
l
y
pr
one
t
o
fl
oodi
ng
m
a
y
be
com
e
l
e
s
s
s
o.
H
ow
e
v
e
r
,
t
he
ov
e
r
a
l
l
i
m
pa
ct
f
or
ne
a
r
l
y
a
l
l
popul
a
t
i
ons
a
nd
f
or
t
he
w
or
l
d
a
s
a
w
hol
e
is
e
x
pe
ct
e
d t
o b
e
mor
e
ne
ga
t
iv
e
t
h
a
n pos
it
iv
e
, in
cr
e
a
s
ingly
s
o a
s
clima
t
e
cha
n
ge
pr
ogr
e
s
s
e
s
. In a
d
dit
ion, t
he
la
t
it
ude
r
a
n
g
e
i
n
t
h
e
w
o
r
l
d
t
ha
t
m
a
y
b
e
ne
fi
t
f
r
o
m
l
e
s
s
c
o
l
d
(e
.
g
.
,
t
h
e
f
a
r
n
or
t
h
o
f
t
h
e
N
o
r
t
he
r
n
H
e
m
i
s
p
he
r
e
)
ha
s
f
e
w
e
r
i
nha
bi
t
a
nt
s
com
pa
r
e
d
w
i
t
h
t
he
e
qua
t
or
i
a
l
l
a
t
i
t
ude
s
w
he
r
e
t
he
bur
de
n
w
i
l
l
be
gr
e
a
t
e
s
t
.
Fr
e
que
nt
l
y
As
k
e
d
Q
ue
s
t
i
ons
FAQ 11.3 | Who is most af
fected by climate change?
W
hi
l
e
t
he
di
r
e
ct
he
a
l
t
h
e
ff
e
ct
s
of
e
x
t
r
e
m
e
w
e
a
t
he
r
e
v
e
nt
s
r
e
ce
i
v
e
gr
e
a
t
a
t
t
e
nt
i
on,
cl
i
m
a
t
e
cha
nge
m
a
i
nl
y
ha
r
m
s
hum
a
n he
a
l
t
h by
e
x
a
ce
r
ba
t
i
ng e
x
i
s
t
i
ng di
s
e
a
s
e
bur
de
ns
a
nd ne
ga
t
i
v
e
i
m
pa
ct
s
on da
i
l
y
l
i
f
e
a
m
ong t
hos
e
w
i
t
h t
he
w
e
a
k
e
s
t
he
a
l
t
h pr
ot
e
ct
i
on s
y
s
t
e
m
s
,
a
nd w
i
t
h t
he
l
e
a
s
t
ca
pa
ci
t
y
t
o a
da
pt
.
T
hus
,
m
os
t
a
s
s
e
s
s
m
e
nt
s
i
ndi
ca
t
e
t
ha
t
poor
and
di
senfranchi
sed
groups
wi
l
l
bear
the
m
ost
ri
sk
and,
gl
obal
l
y
,
the
greatest
burden
wi
l
l
fal
l
on
poor
countri
es,
parti
cul
arl
y
on
poor
chi
l
dren,
who
are
m
ost
affected
today
by
such
cl
i
m
ate-rel
ated
di
seases
as
m
al
ari
a,
undernutri
ti
on,
a
nd dia
rrhe
a
. H
owe
v
e
r
, the
div
e
rse
a
nd globa
l e
ffe
cts of clima
te
cha
nge
me
a
n tha
t highe
r income
popula
tions ma
y
al
so
be
affected
by
ex
trem
e
ev
ents,
em
ergi
ng
ri
sks,
and
the
spread
of
i
m
pacts
from
m
ore
v
ul
nerabl
e
popul
ati
ons.
Fr
equent
l
y
As
ked
Ques
t
i
ons
FAQ 11.4 | What is the most important adaptation strategy
to reduce the health impacts of climate change?
I
n
the
i
m
m
edi
ate
future,
ac
c
el
erati
ng
publ
i
c
heal
th
and
m
edi
c
al
i
nterv
enti
ons
to
reduc
e
the
present
burden
of
di
sease,
parti
cul
arl
y
di
seases
i
n
poor
countri
es
rel
ated
to
cl
i
m
ati
c
condi
ti
ons,
i
s
the
si
ngl
e
m
ost
i
m
portant
step
that
ca
n be
take
n to re
duce
the hea
l
th i
m
pa
cts of cl
i
m
a
te
cha
nge
.
P
ri
ori
ty
i
nte
rv
e
nti
ons i
ncl
ude
i
m
prov
e
d m
a
na
gem
ent
o
f
t
h
e
e
n
vir
o
n
me
n
t
a
l d
e
t
e
r
min
a
n
t
s
o
f
h
e
a
lt
h
(s
u
ch
a
s
p
r
o
vis
io
n
o
f
wa
t
e
r
a
n
d
s
a
n
it
a
t
io
n
),
in
f
e
ct
io
u
s
d
is
e
a
s
e
surv
ei
l
l
ance,
and
strengtheni
ng
the
resi
l
i
ence
of
heal
th
sy
stem
s
to
ex
trem
e
weather
ev
ents.
A
l
l
ev
i
ati
on
of
pov
erty
i
s
al
so
a
necessary
condi
ti
on
for
successful
adaptati
on.
There are l
i
m
i
ts to heal
th adaptati
on,
howev
er
.
F
or ex
am
pl
e,
the hi
gher-
end proj
ecti
ons of warm
i
ng i
ndi
cate that
be
f
or
e
t
he
e
nd of
t
he
2
1
s
t
ce
nt
ur
y, pa
r
t
s
of
t
he
wor
ld ma
y e
xpe
r
ie
nce
t
e
mpe
r
a
t
ur
e
s
t
ha
t
e
xce
e
d phys
iologica
l limit
s
duri
ng
peri
ods
of
the
y
ear
,
m
aki
ng
i
t
i
m
possi
bl
e
to
work
or
carry
out
other
phy
si
cal
acti
v
i
ty
outsi
de.
Fr
equent
l
y
As
ked
Ques
t
i
ons
F
AQ 11.5 | What ar
e health “co-benefits” of climate change mitigation measures?
M
a
ny mitiga
tion me
a
sures tha
t re
duc
e e
missions of those climate-altering pollutants (CAPs) that warm the planet
have importa
nt direc
t he
alth be
ne
fi
ts in a
ddition to reducing the risk of climate change. This relationship is called
“co-ben
efits.” For example, in
creasin
g combustion efficiency in households cooking with biomass or coal could
ha
ve
clima
te be
ne
fi
ts
by re
ducing CAP
s a
nd a
t the same time bring major health benefits among poor populations.
Ene
r
gy e
f
fici
ency a
nd r
educi
ng r
e
l
i
a
nce
on coal for electricity generation not only reduces emissions of greenhouse
gas
es
,
but
a
l
s
o r
educes
e
m
i
s
s
i
ons
of
fine pa
r
ticles that cause many premature deaths worldwide as well as reducing
other
he
a
lth
impa
c
ts
from
the
c
oa
l
fuel
c
yc
le
. Programs that encourage “active transport” (walking and cycling) in
place of travel by motor vehicle reduc
e both CAP emissions and offer direct health benefits. A major share of
greenhouse gas emissions from the food and agriculture sector arises from cows, goats, and sheep—ruminants that
create the greenhouse gas methane as part of their digestive process. Reducing consumption of meat and dairy
products from these animals may reduce ischemic heart disease (assuming replacement with plant-based
polyunsaturates) and some types of cancer. Programs to provide access to reproductive health services for all women
will not only lead to slower population growth and its associated energy demands, but also will reduce the numbers
of child and maternal deaths.

743
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
References
Abuaku, B.K., J. Zhou, X. Li, S. Li, A. Liu, T. Yang, and H. Tan, 2009: Morbidity and
mortality among populations suffering floods in Hunan, China: the role of
socioeconomic status. Journal of Flood Risk Management, 2(3), 222-228.
Acosta-Michlik, L., U. Kelkar, and U. Sharma, 2008: A critical overview: local evidence
on vulnerabilities and adaptations to global environmental change in developing
countries. Global Environmental Change, 18(4), 539-542.
Ahern, M.J., R.S. Kovats, P. Wilkinson, R. Few, and F. Matthies, 2005: Global health
impacts of floods: epidemiological evidence. Epidemiologic Reviews, 27, 36-
45.
Albrecht, G., G.M. Sartore, L. Connor, N. Higginbotham, S. Freeman, B. Kelly, H. Stain,
A. Tonna, and G. Pollard, 2007: Solastalgia: the distress caused by environmental
change. Australasian Psychiatry, 15 (Suppl. 1), S95-S98.
Alderman, H., 2010: Safety nets can help address the risks to nutrition from increasing
climate variability. The Journal of Nutrition, 140(Suppl. 1), 148S-152S.
Alexander, K.A., M. Carzolio, D. Goodin, and E. Vance, 2013: Climate change is likely
to worsen the public health threat of diarrheal disease in Botswana.
International Journal of Environmental Research and Public Health, 10(4),
1202-1230.
Alonso, D., M.J. Bouma, and M. Pascual, 2011: Epidemic malaria and warmer
temperatures in recent decades in an East African highland. Proceedings of the
Royal Society B, 278(1712), 1661-1669.
Alston, M. and J. Kent, 2008: The Big Dry: the link between rural masculinities and
poor health outcomes for farming men. Journal of Sociology, 44(2), 133-147.
Altizer, S., A. Dobson, P. Hosseini, P. Hudson, M. Pascual, and P. Rohani, 2006:
Seasonality and the dynamics of infectious diseases. Ecology Letters, 9(4), 467-
484.
Analitis, A., I. Georgiadis, and K. Katsouyanni, 2012: Forest fires are associated with
elevated mortality in a dense urban setting. Occupational Environmental
Medicine, 69(3), 158-162.
Anderson, G.B. and M.L. Bell, 2011: Heat waves in the United States: mortality risk
during heat waves and effect modification by heat wave characteristics in 43
U.S. communities. Environmental Health Perspectives, 119(2), 210-218.
Anderson, G.B. and M.L. Bell, 2012: Lights out: impact of the August 2003 power
outage on mortality in New York, NY. Epidemiology, 23(2), 189-193.
Anderson, K. and A. Bows, 2011: Beyond ‘dangerous’ climate change: emission
scenarios for a new world. Philosophical Transactions of the Royal Society A,
369(1934), 20-44.
Anderson, M., C. Carmichael, V. Murray, A. Dengel, and M. Swainson, 2012: Defining
indoor heat thresholds for health in the UK. Perspectives in Public Health,
133(3), 158-164.
Andreassen, A., S. Jore, P. Cuber, S. Dudman, T. Tengs, K. Isaksen, H. Hygen, H.
Viljugrein, G. Anestad, P. Ottesen, and K. Vainio, 2012: Prevalence of tick borne
encephalitis virus in tick nymphs in relation to climatic factors on the southern
coast of Norway. Parasites & Vectors, August 2012, 5, 177, doi:10.1186/1756-
3305-5-177.
Andriopoulos, P., A. Economopoulou, and G. Spanakos, 2013: A local outbreak of
autochthonous Plasmodium vivax malaria in Laconia, Greece – a re-emerging
infection in the southern borders of Europe? International Journal of Infectious
Disease, 17(2), e125-e128.
Anenberg, S.C., J. Schwartz, D. Shindell, M. Amann, G. Faluvegi, Z. Klimont, G.
Janssens-Maenhout, L. Pozzoli, R. van Dingenen, E. Vignati, L. Emberson, N.Z.
Muller, J.J. West, M. Williams, V. Demkine, W.K. Hicks, J. Kuylenstierna, F. Raes,
and V. Ramanathan, 2012: Global air quality and health co-benefits of mitigating
near-term climate change through methane and black carbon emission controls.
Environmental Health Perspectives, 120(6), 831-839.
Anenberg, S.C., K. Balakrishnan, J. Jetter, O. Masera, S. Mehta, J. Moss, and V.
Ramanathan, 2013: Cleaner cooking solutions to achieve health, climate, and
economic cobenefits. Environmental Science & Technology, 47(9), 3944-3952.
Angelini, P., P. Macini, A.C. Finarelli, C. Pol, C. Venturelli, R. Bellini, and M. Dottori,
2008: Chikungunya epidemic outbreak in Emilia-Romagna (Italy) during summer
2007. Parassitologia, 50(1-2), 97-98.
Anyamba, A., K.J. Linthicum, and J.L. Small, 2012: Climate teleconnections and recent
patterns of human and animal disease outbreaks. PLoS Neglected Tropical
Diseases, 6(1), e1465, doi:10.1371/journal.pntd.0001465.
Apsimon, H., M. Amann, S. Astrom, and T. Oxley, 2009: Synergies in addressing air
quality and climate change. Climate Policy, 9(6), 669-680.
Ari, T.B., A. Gershunov, R. Tristan, B. Cazelles, K. Gage, and N.C. Stenseth, 2010:
Interannual variability of human plague occurrence in the western United
States explained by tropical and North Pacific Ocean climate variability. The
American Journal of Tropical Medicine and Hygiene, 83(3), 624-632.
Astrom, C., J. Rocklov, S. Hales, A. Beguin, V. Louis, and R. Sauerborn, 2012: Potential
distribution of dengue fever under scenarios of climate change and economic
development. Ecohealth, 9(4), 448-454.
Atchison, C., M. Iturriza-Gomara, C. Tam, and B. Lopman, 2010: Spatiotemporal
dynamics of rotavirus disease in Europe: can climate or demographic variability
explain the patterns observed. The Pediatric Infectious Disease Journal, 29(6),
566-568.
Auffhammer, M., 2011: Agriculture: weather dilemma for African maize. Nature
Climate Change, 1, 27-28.
Babey, S.H., T.A. Hastert, and E.R. Brown, 2007: Teens Living in Disadvantaged
Neighborhoods Lack Access to Parks and Get Less Physical Activity. Policy Brief,
Center for Health Policy Research, University of California, Los Angeles (UCLA),
Los Angeles, CA, USA, 6 pp.
Babey, S.H., T.A. Hastert, H. Yu, and E.R. Brown, 2008: Physical activity among
adolescents. When do parks matter? American Journal of Preventive Medicine,
34(4), 345-348.
Baccini, M., T. Kosatsky, A. Analitis, H.R. Anderson, M. D’Ovidio, B. Menne, P. Michelozzi,
A. Biggeri, and P.C. Grp, 2011: Impact of heat on mortality in 15 European cities:
attributable deaths under different weather scenarios. Journal of Epidemiology
and Community Health, 65(1), 64-70.
Bai, L., L.C. Morton, and Q. Liu, 2013: Climate change and mosquito-borne diseases
in China: a review. Globalization and Health, 9(1), 10, doi:10.1186/1744-8603-
9-10.
Bandyopadhyay, S., S. Kanji, and L. Wang, 2012: The impact of rainfall and temperature
variation on diarrheal prevalence in sub-Saharan Africa. Applied Geography,
33, 63-72.
Bangs, M.J., R.P. Larasati, A.L. Corwin, and S. Wuryadi, 2006: Climatic factors associated
with epidemic dengue in Palembang, Indonesia: implications of short-term
meteorological events on virus transmission. Southeast Asian Journal of Tropical
Medicine and Public Health, 37(6), 1103-1116.
Bassil, K. and D. Cole, 2010: Effectiveness of public health interventions in reducing
morbidity and mortality during heat episodes: a structured review. International
Journal of Environmental Research and Public Health, 7(3), 991-1001.
Basu, R. and B.D. Ostro, 2008: A multicounty analysis identifying the populations
vulnerable to mortality associated with high ambient temperature in California.
American Journal of Epidemiology, 168(6), 632-637.
Battisti, D.S. and R.L. Naylor, 2009: Historical warnings of future food insecurity with
unprecedented seasonal heat. Science, 323(5911), 240-244.
Baumgartner, J., J.J. Schauer, M. Ezzati, L. Lu, C. Cheng, J.A. Patz, and L.E. Bautista,
2011: Indoor air pollution and blood pressure in adult women living in rural
China. Environmental Health Perspectives, 119(10), 1390-1395.
Beaglehole, R. and R. Bonita, 2008: Global public health: a scorecard. Lancet,
372(9654), 1988-1996.
Beebe, N.W., R.D. Cooper, P. Mottram, and A.W. Sweeney, 2009: Australia’s dengue
risk driven by human adaptation to climate change. PLoS Neglected Tropical
Diseases, 3(5), e429, doi:10.1371/journal.pntd.0000429.
Beggs, P.J., 2010: Adaptation to impacts of climate change on aeroallergens and
allergic respiratory diseases. International Journal of Environmental Research
and Public Health, 7(8), 3006-3021.
Béguin, A., S. Hales, J. Rocklöv, C. Åström, V.R. Louis, and R. Sauerborn, 2011: The
opposing effects of climate change and socio-economic development on the
global distribution of malaria. Global Environmental Change, 21(4), 1209-1214.
Bélanger, M., K. Gray-Donald, J. O’Loughlin, G. Paradis, and J. Hanley, 2009: Influence
of weather conditions and season on physical activity in adolescents. Annals
of Epidemiology, 19(3), 180-6, doi: 10.1016/j.annepidem.2008.12.008.
Bell, M.L., R.D. Peng, and F. Dominici, 2006: The exposure-response curve for ozone
and risk of mortality and the adequacy of current ozone regulations.
Environmental Health Perspectives, 114(4), 532-536.
Bell, M.L., R. Goldberg, C. Hogrefe, P. Kinney, K. Knowlton, B. Lynn, J. Rosenthal, C.
Rosenzweig, and J. Patz, 2007: Climate change, ambient ozone, and health in
50 US cities. Climatic Change, 82(1), 61-76.
Bell, M.L., D.L. Davis, L.A. Cifuentes, A.J. Krupnick, R.D. Morgenstern, and G.D.
Thurston, 2008a: Ancillary human health benefits of improved air quality
resulting from climate change mitigation. Environmental Health, 7, 41,
doi:10.1186/1476-069X-7-41.

744
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Bell, M.L., M.S. O’Neill, N. Ranjit, V.H. Borja-Aburto, L.A. Cifuentes, and N.C. Gouveia,
2008b: Vulnerability to heat-related mortality in Latin America: a case-crossover
study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. International
Journal of Epidemiology, 37(4), 796-804.
Bennet, L., A. Halling, and J. Berglund, 2006: Increased incidence of Lyme borreliosis
in southern Sweden following mild winters and during warm, humid summers.
European Journal of Clinical Microbiology & Infectious Diseases, 25(7), 426-
432.
Bennett, C.M. and A.J. McMichael, 2010: Non-heat related impacts of climate
change on working populations. Global Health Action, 3, 5460, doi:10.3402/
gha.v3i0.5640.
Bennett, C.M., K.G. Dear, and A. McMichael, 2013: Shifts in the seasonal distribution
of deaths in Australia, 1968-2007. International Journal of Biometeorology,
(April), doi:10.1007/s00484-013-0663-x.
Berry, H.L., 2007: “Crowded suburbs” and “killer cities”: a brief review of the
relationship between the urban environment and mental health. New South
Wales Public Health Bulletin, 18(11-12), 222-227.
Berry, H.L., K. Bowen, and T. Kjellstrom, 2010: Climate change and mental health: a
causal pathways framework. International Journal of Public Health, 55(2), 123-
132.
Bhatt, S., P.W. Gething, O.J. Brady, J.P. Messina, A.W. Farlow, C.L. Moyes, J.M. Drake,
J.S. Brownstein, A.G. Hoen, O. Sankoh, M.F. Myers, D.B. George, T. Jaenisch,
G.R.W. Wint, C.P. Simmons, T.W. Scott, J.J. Farrar, and S.I. Hay, 2013: The global
distribution and burden of dengue. Nature, 496(7446), 504-507.
Bi, P. and K.A. Parton, 2008: Effect of climate change on Australian rural and remote
regions: what do we know and what do we need to know? Australian Journal
of Rural Health, 16(1), 2-4.
Bi, P., Y. Zhang, and K.A. Parton, 2007: Weather variables and Japanese encephalitis
in the metropolitan area of Jinan city, China. Journal of Infection, 55(6), 551-
556.
Black, R.E., L.H. Allen, Z.A. Bhutta, L.E. Caulfield, M.d. Onis, M. Ezzati, C. Mathers,
and J. Rivera, 2008: Maternal and child undernutrition: global and regional
exposures and health consequences. Lancet, 371(9608), 243-260.
Boldo, E., C. Linares, J. Lumbreras, R. Borge, A. Narros, J. García-Pérez, P. Fernández-
Navarro, B. Pérez-Gómez, N. Aragonés, R. Ramis, M. Pollán, T. Moreno, A.
Karanasiou, and G. López-Abente, 2010: Health impact assessment of a
reduction in ambient PM
2.5
levels in Spain. Environment International, 37(2),
342-348.
Bompangue, N.D., P. Giraudoux, P.D. Plisnier, T.A. Mutombo, M. Piarroux, and B. Sudre,
2011: Dynamics of cholera outbreaks in Great Lakes region of Africa, 1978-
2008. Emerging Infectious Diseases, 17(11), 2026-2034.
Bond, T.C., S.J. Doherty, D.W. Fahey, P.M. Forster, T. Berntsen, B.J. DeAngelo, M.G.
Flanner, S. Ghan, B. Kärcher, D. Koch, S. Kinne, Y. Kondo, P.K. Quinn, M.C. Sarofim,
M.G. Schultz, M. Schulz, C. Venkataraman, H. Zhang, S. Zhang, N. Bellouin, S.K.
Guttikunda, P.K. Hopke, M.Z. Jacobson, J.W. Kaiser, Z. Klimont, U. Lohmann, J.P.
Schwarz, D. Shindell, T. Storelvmo, S.G. Warren, and C.S. Zender, 2013: Bounding
the role of black carbon in the climate system: a scientific assessment. Journal
of Geophysical Research: Atmospheres, 118(11), 5380-5552.
Bonjour, S., H. Adair-Rohani, J. Wolf, S. Mehta, A. Pruss-Ustun, M. Lahiff, E.A. Rehfuess,
V. Mishra, and K.R. Smith, 2013: Solid fuel use for household cooking: country
and regional estimates for 1980-2010. Environmental Health Perspectives,
121(7), 784-790.
Bonovas, S. and G. Nikolopoulos, 2012: High-burden epidemics in Greece in the era
of economic crisis. Early signs of a public health tragedy. Journal of Preventive
Medicine and Hygiene, 53(3), 169-171.
Bouchama, A., M. Dehbi, G. Mohamed, F. Matthies, M. Shoukri, and B. Menne, 2007:
Prognostic factors in heat wave related deaths: a meta-analysis. Archives of
Internal Medicine, 167(20), 2170-2176.
Bowen, K.J., S. Friel, K. Ebi, C.D. Butler, F. Miller, and A.J. McMichael, 2012: Governing
for a healthy population: towards an understanding of how decision-making
will determine our global health in a changing climate. International Journal
of Environmental Research and Public Health, 9(1), 55-72.
Brázdil, R., M. Trnka, P. Dobrovolný, K. Chromá, P. Hlavinka, and Z. Žalud, 2009:
Variability of droughts in the Czech Republic, 1881-2006. Theoretical and
Applied Climatology, 97(3-4), 297-315.
Breton, M., M. Garneau, I. Fortier, F. Guay, and J. Louis, 2006: Relationship between
climate, pollen concentrations of Ambrosia and medical consultations for
allergic rhinitis in Montreal, 1994-2002. Science of the Total Environment,
370(1), 39-50.
Brouwer, R., S. Akter, L. Brander, and E. Haque, 2007: Socioeconomic vulnerability
and adaptation to environmental risk: a case study of climate change and
flooding in Bangladesh. Risk Analysis, 27(2), 313-326.
Browning, C.R., D. Wallace, S.L. Feinberg, and K.A. Cagney, 2006: Neighborhood social
processes, physical conditions, and disaster-related mortality: the case of the
1995 Chicago heat wave. American Sociological Review, 71(4), 661-678.
Bruce, N., M. Dherani, J. Das, K. Balakrishnan, H. Adair-Rohani, Z. Bhutta, and D. Pope,
2013: Control of household air pollution for child survival: estimates for
intervention impacts. BMC Public Health, 13(Suppl. 3), S8, doi:10.1186/1471-
2458-13-S3-S8.
Brunkard, J., G. Namulanda, and R. Ratard, 2008: Hurricane Katrina deaths,
Louisiana, 2005. Disaster Medicine and Public Health Preparedness, 2(4), 215-
223.
Bujold, E., S.H. Mehta, C. Bujold, and R.J. Gauthier, 2002: Interdelivery interval and
uterine rupture. American Journal of Obstetrics and Gynecology, 187(5), 1199-
1202.
Bulto, P., A.P. Rodriguez, A.R. Valencia, N.L. Vega, M.D. Gonzalez, and A.P. Carrera,
2006: Assessment of human health vulnerability to climate variability and
change in Cuba. Environmental Health Perspectives, 114(12), 1942-1949.
Byass, P., 2010: The imperfect world of global health estimates. PLoS Medicine, 7(11),
e1001006, doi:10.1371/journal.pmed.1001006.
Caminade, C., J.A. Ndione, C.M.F. Kebe, A.E. Jones, S. Danuor, S. Tay, Y.M. Tourre, J.
Lacaux, C. Vignolles, J.B. Duchemin, I. Jeanne, and A.P. Morse, 2011: Mapping
Rift Valley fever and malaria risk over West Africa using climatic indicators.
Atmospheric Science Letters, 12(1), 96-103.
Caminade, C., J.M. Medlock, E. Ducheyne, K.M. McIntyre, S. Leach, M. Baylis, and
A.P. Morse, 2012: Suitability of European climate for the Asian tiger mosquito
Aedes albopictus: recent trends and future scenarios. Journal of the Royal
Society Interface, 9(75), 2708-2717.
Campbell, J.D., M.A. Taylor, T.S. Stephenson, R.A. Watson, and F.S. Whyte, 2011: Future
climate of the Caribbean from a regional climate model. International Journal
of Climatology, 31(12), 1866-1878.
Casagrande, S.S., M.C. Whitt-Glover, K.J. Lancaster, A.M. Odoms-Young, and T.L. Gary,
2009: Built environment and health behaviors among African Americans: a
systematic review. American Journal of Preventive Medicine, 36(2), 174-181.
Casimiro, E., J. Calheiros, F.D. Santos, and R.S. Kovats, 2006: National assessment of
health effects of climate change in Portugal: approach and key findings.
Environmental Health Perspectives, 114(12), 1950-1956.
Chadee, D.D., 2009: Dengue cases and Aedes aegypti indices in Trinidad, West Indies.
Acta Tropica, 112(2), 174-180.
Chadee, D.D., B. Shivnauth, S.C. Rawlins, and A.A. Chen, 2007: Climate, mosquito
indices and the epidemiology of dengue fever in Trinidad (2002-2004). Annals
of Tropical Medicine and Parasitology, 101(1), 69-77.
Chang, H.H., J. Zhou, and M. Fuentes, 2010: Impact of climate change on ambient
ozone level and mortality in southeastern United States. International Journal
of Environmental Research and Public Health, 7(7), 2866-2880.
Chang, Y.K., C.C. Wu, L.T. Lee, R.S. Lin, Y.H. Yu, and Y.C. Chen, 2012: The short-term
effects of air pollution on adolescent lung function in Taiwan. Chemosphere,
87(1), 26-30.
Chapman, R.S., X. He, A.E. Blair, and Q. Lan, 2005: Improvement in household stoves
and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective
cohort study. BMJ, 331, 1050, doi:10.1136/bmj.38628.676088.55.
Chau, P.H., K.C. Chan, and J. Woo, 2009: Hot weather warning might help to reduce
elderly mortality in Hong Kong. International Journal of Biometeorology, 53(5),
461-468.
Chaves, L.F. and C.J. Koenraadt, 2010: Climate change and highland malaria: fresh
air for a hot debate. Quarterly Review of Biology, 85(1), 27-55.
Chaves, L.F., A. Satake, M. Hashizume, and N. Minakawa, 2012: Indian Ocean Dipole
and rainfall drive a Moran effect in East Africa malaria transmission. Journal
of Infectious Diseases, 205(12), 1885-1891.
Cheng, C.H., S.F. Huang, and H.J. Teoh, 2011: Predicting daily ozone concentration
maxima using fuzzy time series based on a two-stage linguistic partition
method. Computers & Mathematics with Applications, 62(4), 2016-2028.
Chowell, G., C.A. Torre, C. Munayco-Escate, L. Suárez-Ognio, R. López-Cruz, J.M.
Hyman, and C. Castillo-Chavez, 2008: Spatial and temporal dynamics of dengue
fever in Peru: 1994-2006. Epidemiology & Infection, 136(12), 1667-77.
Chowell, G., B. Cazelles, H. Broutin, and C.V. Munayco, 2011: The influence of
geographic and climate factors on the timing of dengue epidemics in Perú,
1994-2008. BMC Infectious Diseases, 11, 164, doi:10.1186/1471-2334-11-164.

745
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
Christidis, N., P.A. Stott, G.S. Jones, H. Shiogama, T. Nozawa, and J. Luterbacher, 2012:
Human activity and anomalously warm seasons in Europe. International Journal
of Climatology, 32(2), 225-239.
Cleary-Goldman, J., F.D. Malone, J. Vidaver, R.H. Ball, D.A. Nyberg, C.H. Comstock,
G.R. Saade, K.A. Eddleman, S. Klugman, L. Dugoff, I.E. Timor-Tritsch, S.D. Craigo,
S.R. Carr, H.M. Wolfe, D.W. Bianchi, and M. D’Alton, 2005: Impact of maternal
age on obstetric outcome. Obstetrics & Gynecology, 105(5 Pt. 1), 983-990.
Cohen, J.E., 2010: Population and climate change. Proceedings of the American
Philosophical Society, 154(2), 158-182.
Conde-Agudelo, A., A. Rosas-Bermúdez, and A.C. Kafury-Goeta, 2007: Effects of
birth spacing on maternal health: a systematic review. American Journal of
Obstetrics and Gynecology, 196(4), 297-308.
Cook, J.T. and D.A. Frank, 2008: Food security, poverty, and human development in
the United States. Annals of the New York Academy of Sciences, 1136(1), 193-
209.
Cook, S.M., R.I. Glass, C.W. LeBaron, and M.S. Ho, 1990: Global seasonality of
rotavirus infections. Bulletin of the World Health Organization, 68(2), 171-177.
Correa, M.d.P., S. Godin-Beekmann, M. Haeffelin, S. Bekki, P. Saiag, J. Badosa, F. Jegou,
A. Pazmino, and E. Mahe, 2013: Projected changes in clear-sky erythemal and
vitamin D effective UV doses for Europe over the period 2006 to 2100.
Photochemical & Photobiological Sciences, 12(6), 1053-1064.
Danis, K., A. Baka, A. Lenglet, W. Van Bortel, I. Terzaki, M. Tseroni, M. Detsis, E.
Papanikolaou, A. Balaska, S. Gewehr, G. Dougas, T. Sideroglou, A. Economopoulou,
N. Vakalis, S. Tsiodras, S. Bonovas, and J. Kremastinou, 2011: Autochthonous
Plasmodium vivax malaria in Greece, 2011. Eurosurveillance, 16(42), www.
eurosurveillance.org/images/dynamic/EE/V16N42/art19993.pdf.
Dasgupta, S., B. Laplante, S. Murray, and D. Wheeler, 2009: Climate Change and the
Future Impacts of Storm-Surge Disasters in Developing Countries. Working
Paper 182, Center for Global Development (CDG), Washington, DC, USA, 22 pp.
Davis, T.W., D.L. Berry, G.L. Boyer, and C.J. Gobler, 2009: The effects of temperature
and nutrients on the growth and dynamics of toxic and non-toxic strains of
Microcystis during cyanobacteria blooms. Harmful Algae, 8(5), 715-725.
De Haen, H. and G. Hemrich, 2007: The economics of natural disasters: implications
and challenges for food security. Agricultural Economics, 37, 31-45.
de Magny, G.C., R. Murtugudde, M.R.P. Sapiano, A. Nizam, C.W. Brown, A.J. Busalacchi,
M. Yunus, G.B. Nair, A.I. Gil, C.F. Lanata, J. Calkins, B. Manna, K. Rajendran, M.K.
Bhattacharya, A. Huq, R.B. Sack, and R.R. Colwell, 2008: Environmental signatures
associated with cholera epidemics. Proceedings of the National Academy of
Sciences of the United States of America, 105(46), 17676-17681.
Dear, K., G. Ranmuthugala, T. Kjellstrom, C. Skinner, and I. Hanigan, 2005: Effects of
temperature and ozone on daily mortality during the August 2003 heat wave
in France. Archives of Environmental & Occupational Health, 60(4), 205-212.
Delatte, H., G. Gimonneau, A. Triboire, and D. Fontenille, 2009: Influence of temperature
on immature development, survival, longevity, fecundity, and gonotrophic cycles
of Aedes albopictus, vector of chikungunya and dengue in the Indian Ocean.
Journal of Medical Entomology, 46(1), 33-41.
Delpla, I., A.V. Jung, E. Baures, M. Clement, and O. Thomas, 2009: Impacts of climate
change on surface water quality in relation to drinking water production.
Environment International, 35(8), 1225-1233.
Dennekamp, M. and M. Carey, 2010: Air quality and chronic disease: why action on
climate change is also good for health. New South Wales Public Health Bulletin,
21(5-6), 115-121.
Descloux, E., M. Mangeas, C.E. Menkes, M. Lengaigne, A. Leroy, T. Tehei, L. Guillaumot,
M. Teurlai, A.C. Gourinat, J. Benzler, A. Pfannstiel, J.P. Grangeon, N. Degallier,
and X. De Lamballerie, 2012: Climate-based models for understanding and
forecasting dengue epidemics. PLoS Neglected Tropical Diseases, 6(2), e1470,
doi:10.1371/journal.pntd.0001470.
Dey, S.K., H. Ushijima, O. Phathammavong, W. Chanit, S. Okitsu, M. Mizuguchi, and
Y. Ota, 2010: Seasonal trend and serotype distribution of rotavirus infection in
Japan, 1981-2008. The Pediatric Infectious Disease Journal, 29(2), 166-167.
Diamond-Smith, N. and M. Potts, 2011: A woman cannot die from a pregnancy she
does not have. International Perspectives on Sexual and Reproductive Health,
37(3), 155-157.
Diboulo, E., A. Sie, J. Rocklov, L. Niamba, M. Ye, C. Bagagnan, and R. Sauerborn, 2012:
Weather and mortality: a 10 year retrospective analysis of the Nouna Health
and Demographic Surveillance System, Burkina Faso. Global Health Action,
5(Suppl. 1), 19078, doi:10.3402/gha.v5i0.19078.
Diffenbaugh, N. and F. Giorgi, 2012: Climate change hotspots in the CMIP5 global
climate model ensemble. Climatic Change, 114(3-4), 813-822.
D’Ippoliti, D., P. Michelozzi, C. Marino, F. de’Donato, B. Menne, K. Katsouyanni, U.
Kirchmayer, A. Analitis, M. Medina-Ramón, A. Paldy, R. Atkinson, S. Kovats, L.
Bisanti, A. Schneider, A. Lefranc, C. Iñiguez, and C.A. Perucci, 2010: The impact
of heat waves on mortality in 9 European cities: results from the EuroHEAT
project. Environmental Health, 9, 37, doi:10.1186/1476-069X-9-37.
Dix-Cooper, L., B. Eskenazi, C. Romero, J. Balmes, and K.R. Smith, 2012: Neuro-
developmental performance among school age children in rural Guatemala is
associated with prenatal and postnatal exposure to carbon monoxide, a marker
for exposure to woodsmoke. Neurotoxicology, 33(2), 246-254.
Dodman, D., D. Mitlin, and J.C. Rayos Co, 2010: Victims to victors, disasters to
opportunities: community-driven responses to climate change in the Philippines.
International Development Planning Review, 32(1), 1-26, doi:10.3828/idpr.2009.10.
Dong, G.H., T. Chen, M.M. Liu, D. Wang, Y.N. Ma, W.H. Ren, Y.L. Lee, Y.D. Zhao, and
Q.C. He, 2011: Gender differences and effect of air pollution on asthma in
children with and without allergic predisposition: northeast Chinese children
health study. PLoS One, 6(7), e22470, doi:10.1371/journal.pone.0022470.
Doocy, S., A. Daniels, S. Murray, and T.D. Kirsch, 2013: The human impact of floods:
a historical review of events 1980-2009 and systematic literature review. PLOS
Currents Disasters, 2013 April 16, Edition 1, doi:10.1371/currents.dis.
f4deb457904936b07c09daa98ee8171a.
Dossou, K. and B. Glehouenou-Dossou, 2007: The vulnerability to climate change of
Cotonou (Benin): the rise in sea level. Environment and Urbanization, 19, 65-79.
Doyon, B., D. Belanger, and P. Gosselin, 2008: The potential impact of climate change
on annual and seasonal mortality for three cities in Quebec, Canada. International
Journal of Health Geographics, 7, 23, doi:10.1186/1476-072X-7-23.
Dunne, J., R. Stouffer, and J. John, 2013: Reductions in labour capacity from heat stress
under climate warming. Nature Climate Change, 3(3), 563-566, doi:10.1038/
nclimate1827.
Durand, C.P., M. Andalib, G.F. Dunton, J. Wolch, and M.A. Pentz, 2011: A systematic
review of built environment factors related to physical activity and obesity risk:
implications for smart growth urban planning. Obesity Reviews, 12(5), e173-
82, doi:10.1111/j.1467-789X.2010.00826.x.
Earnest, A., S.B. Tan, and A. Wilder-Smith, 2012: Meteorological factors and El Nino
Southern Oscillation are independently associated with dengue infections.
Epidemiology & Infection, 140(7), 1244-1251.
Ebi, K.L. and G. McGregor, 2008: Climate change, tropospheric ozone and particulate
matter, health impacts. Environmental Health Perspectives, 116(11), 1449-1455.
Ebi, K.L. and D. Mills, 2013: Winter mortality in a warming world: a re-assessment.
WIREs Climate Change, 4, 203-212.
Ebi, K.L., K.A. Exuzides, E. Lau, M. Kelsh, and A. Barnston, 2004: Weather changes
associated with hospitalizations for cardiovascular diseases and stroke in
California, 1983-1998. International Journal of Biometeorology, 49(1), 48-58.
Ebi, K.L., J. Smith, I. Burton, and J. Scheraga, 2006: Some lessons learned from public
health on the process of adaptation. Mitigation Adaptation Strategies Global
Change, 11, 607-620.
Edwards, R.D., K.R. Smith, J. Zhang, and Y. Ma, 2004: Implications of changes in
household stoves and fuel use in China. Energy Policy, 32(3), 395-411.
Engelman, R., 2010: Population, Climate Change, and Women’s Lives. Worldwatch
Report No.183, Worldwatch Institute, Washington, DC, USA, 44 pp.
EPA, 2010: Air Quality Trends. United States Environmental Protection Agency (EPA),
Washington, DC, USA, last updated September 3, 2013, www.epa.gov/airtrends/
aqtrends.html.
Erdner, D.L., J. Dyble, M.L. Parsons, R.C. Stevens, K.A. Hubbard, M.L. Wrabel, S.K.
Moore, K.A. Lefebvre, D.M. Anderson, P. Bienfang, R.R. Bidigare, M.S. Parker, P.
Moeller, L.E. Brand, and V.L. Trainer, 2008: Centers for Oceans and Human
Health: a unified approach to the challenge of harmful algal blooms.
Environmental Health, 7 (Suppl. 2), S2, www.ehjournal.net/content/7/S2/S2.
Estrada-Peña, A., N. Ayllón, and J. de la Fuente, 2012: Impact of climate trends on
tick-borne pathogen transmission. Frontiers in Physiology, 3, 64, doi:10.3389/
fphys.2012.00064.
Ezzine-de-Blas, D., J. Börner, A. Violato-Espada, N. Nascimento, and M. Piketty, 2011:
Forest loss and management in land reform settlements: implications for REDD
governance in the Brazilian Amazon. Environmental Science & Policy, 14(2),
188-200.
Fang, L.Q., X.J. Wang, S. Liang, Y.L. Li, S.X. Song, W.Y. Zhang, Q. Qian, Y.P. Li, L. Wei,
Z.Q. Wang, H. Yang, and W.C. Cao, 2010: Spatiotemporal trends and climatic
factors of hemorrhagic fever with renal syndrome epidemic in Shandong
Province, China. PLoS Neglected Tropical Diseases, 4(8), e789, doi:10.1371/
journal.pntd.0000789.

746
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Feachem, R.G., A.A. Phillips, J. Hwang, C. Cotter, B. Wielgosz, B.M. Greenwood, O.
Sabot, M.H. Rodriguez, R.R. Abeyasinghe, T.A. Ghebreyesus, R.W Snow, 2010:
Shrinking the malaria map: progress and prospects. Lancet, 376(9752), 1566–
1578.
Finlay, S., A. Moffat, R. Gazzard, D. Baker, and V. Murray, 2012: Health impacts of
wildfires. PLoS Currents, 2012 November 2, Edition 1, doi:10.1371/
4f959951cce2c.
Finucane, M.M., G.A. Stevens, M.J. Cowan, G. Danaei, J.K. Lin, C.J. Paciorek, G.M.
Singh, H.R. Gutierrez, Y. Lu, A.N. Bahalim, F. Farzadfar, L.M. Riley, M. Ezzati, and
the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating
Group (Body Mass Index), 2011: National, regional, and global trends in body-
mass index since 1980: systematic analysis of health examination surveys and
epidemiological studies with 960 country-years and 9.1 million participants.
Lancet, 377(9765), 557-567.
Foley, J.A., N. Ramankutty, K.A. Brauman, E.S. Cassidy, J.S. Gerber, M. Johnston, N.D.
Mueller, C. O’Connell, D.K. Ray, P.C. West, C. Balzer, E.M. Bennett, S.R. Carpenter,
J. Hill, C. Monfreda, S. Polasky, J. Rockström, J. Sheehan, S. Siebert, D. Tilman,
and D.P.M. Zaks, 2011: Solutions for a cultivated planet. Nature, 337(7369),
337-342.
Ford, J.D., 2009: Vulnerability of Inuit food systems to food insecurity as a
consequence of climate change: a case study from Igloolik, Nunavut. Regional
Environmental Change, 9(2), 83-100.
Ford, J.D., T. Pearce, J. Gilligan, B. Smit, and J. Oakes, 2008: Climate change and
hazards associated with ice use in northern Canada. Arctic, Antarctic, and
Alpine Research, 40(4), 647-659.
Fouillet, A., G. Rey, F. Laurent, G. Pavillon, S. Bellec, C. Guihenneuc-Jouyaux, J. Clavel,
E. Jougla, and D. Hémon, 2006: Excess mortality related to the August 2003
heat wave in France. International Archives of Occupational & Environmental
Health, 80(1), 16-24.
Fouillet, A., G. Rey, V. Wagner, K. Laaidi, P. Empereur-Bissonnet, A. Le Tertre, P.
Frayssinet, P. Bessemoulin, F. Laurent, P. De Crouy-Chanel, E. Jougla, and D.
Hémon, 2008: Has the impact of heat waves on mortality changed in France
since the European heat wave of summer 2003? A study of the 2006 heat wave.
International Journal of Epidemiology, 37(2), 309-317.
Friel, S., M. Marmot, A.J. McMichael, T. Kjellstrom, and D. Vagero, 2008: Global health
equity and climate stabilisation: a common agenda. Lancet, 372(9650), 1677-
1683.
Friel, S., A.D. Dangour, T. Garnett, K. Lock, Z. Chalabi, I. Roberts, A. Butler, C.D. Butler,
J. Waage, A.J. McMichael, and A. Haines, 2009: Public health benefits of strategies
to reduce greenhouse-gas emissions: food and agriculture. Lancet, 374(9706),
2016-2025.
Frumkin, H. and A.J. McMichael, 2008: Climate change and public health: thinking,
communicating, acting. American Journal of Preventive Medicine, 35(5), 403-
410.
Frumkin, H., J. Hess, G. Luber, J. Malilay, and M. McGeehin, 2008: Climate change:
the public health response. American Journal of Public Health, 98(3), 435-445.
Gamble, J.L., B.J. Hurley, P.A. Schultz, W.S. Jaglom, N. Krishnan, and M. Harris, 2013:
Climate change and older Americans: state of the science. Environmental Health
Perspectives, 121(1), 15-22.
Gasparrini, A. and B. Armstrong, 2011: The impact of heat waves on mortality.
Epidemiology, 22(1), 68-73.
Ge, C., C. Lee, and J. Lee, 2012: The impact of extreme weather events on Salmonella
internalization in lettuce and green onion. Food Research International, 45(2),
1118-1122.
GEA, 2012: Global Energy Assessment – Toward a Sustainable Future. The International
Institute for Applied Systems Analysis (IIASA), Laxenburg, Austria and Cambridge
University Press, Cambridge, UK and New York, NY, USA, 1865 pp.
Gemenne, F., 2011: Climate-induced population displacements in a 4°C+ world.
Philosophical Transactions of the Royal Society A, 369(1934), 182-195.
Gething, P.W., D.L. Smith, A.P. Patil, A.J. Tatem, R.W. Snow, and S.I. Hay, 2010: Climate
change and the global malaria recession. Nature, 465(7296), 342-345.
Gharbi, M., P. Quenel, J. Gustave, S. Cassadou, G. La Ruche, L. Girdary, and L.
Marrama, 2011: Time series analysis of dengue incidence in Guadeloupe, French
West Indies: forecasting models using climate variables as predictors. BMC
Infectious Diseases, 11, 166, doi:10.1186/1471-2334-11-166.
Gosling, S.N., G.R. Mcgregor, and J.A. Lowe, 2009: Climate change and heat-related
mortality in six cities Part 2: climate model evaluation and projected impacts
from changes in the mean and variability of temperature with climate change.
International Journal of Biometeorology, 53(1), 31-51.
Grabow, M.L., S.N. Spak, T. Holloway, B. Stone Jr., A.C. Mednick, and J.A. Patz, 2011:
Air quality and exercise-related health benefits from reduced car travel in
the midwestern United States. Environmental Health Perspectives, 120(1), 68-
76.
Grace, K., F. Davenport, C. Funk, and A.M. Lerner, 2012: Child malnutrition and
climate in sub-Saharan Africa: an analysis of recent trends in Kenya. Applied
Geography, 35(1-2), 405-413.
Gray, J.S., H. Dautel, A. Estrada-Pena, O. Kahl, and E. Lindgren, 2009: Effects of climate
change on ticks and tick-borne diseases in Europe. Interdisciplinary Perspectives
on Infectious Diseases, 2009, 593232, doi:10.1155/2009/593232.
Green, R., L. Cornelsen, A.D. Dangour, R. Turner, B. Shankar, M. Mazzocchi, and R.D.
Smith, 2013: The effect of rising food prices on food consumption: systematic
review with meta-regression. BMJ, 346, f3703, doi:10.1136/bmj.f3703.
Gribble, J.N., N.J. Murray, and E.P. Menotti, 2009: Reconsidering childhood
undernutrition: can birth spacing make a difference? An analysis of the 2002-
2003 El Salvador National Family Health Survey. Maternal & Child Nutrition,
5(1), 49-63.
Gubler, D.J. and G. Kuno, 1997: Dengue and Dengue Haemorrhagic Fever. CAB
International (CABI), Wallingford, UK, 478 pp.
Guha-Sapir, D., F. Vos, and R. Below, 2011: Annual Disaster Statistical Review 2010:
The Numbers and Trends. Center for Research on the Epidemiology of Disasters
(CRED), Université catholique de Louvain, Brussels, Belgium, 42 pp.
Ha, J., H. Kim, and S. Hajat, 2011: Effect of previous-winter mortality on the association
between summer temperature and mortality in South Korea. Environmental
Health Perspectives, 119(4), 542-546.
Haines, A., K.R. Smith, D. Anderson, P.R. Epstein, A.J. McMichael, I. Roberts, P. Wilkinson,
J. Woodcock, and J. Woods, 2007: Policies for accelerating access to clean
energy, improving health, advancing development, and mitigating climate
change. Lancet, 370(9594), 1264-1281.
Haines, A., A. McMichael, K. Smith, I. Roberts, J. Woodcock, A. Markandya, B.
Armstrong, D. Campbell-Lendrum, A. Dangour, M. Davies, N. Bruce, C. Tonne,
M. Barrett, and P. Wilkinson, 2009: Public health benefits of strategies to reduce
greenhouse-gas emissions: overview and implications for policy makers. Lancet,
374(9707), 2104-2114.
Hajat, S., M. O’Connor, and T. Kosatsky, 2010: Health effects of hot weather: from
awareness of risk factors to effective health protection. Lancet, 375(9717),
856-863.
Halide, H. and P. Ridd, 2008: A predictive model for Dengue Hemorrhagic Fever
epidemics. International Journal of Environmental Health, 18(4), 253-265.
Hancock, P., J. Ross, and J. Szalma, 2007: A meta-analysis of performance response
under thermal stressors. Human Factors, 49, 851-877.
Handmer, J., Y. Honda, Z.W. Kundzewicz, N. Arnell, G. Benito, J. Hatfield, I.F. Mohamed,
P. Peduzzi, S. Wu, B. Sherstyukov, and K. Takahashi, 2012: Changes in impacts
of climate extremes: human systems and ecosystems. In: Managing the Risks
of Extreme Events and Disasters to Advance Climate Change Adaptation. A
Special Report of Working Groups I and II of the Intergovernmental Panel on
Climate Change [Field, C.B., V. Barros, T.F. Stocker, D. Qin, D.J. Dokken, K.L. Ebi,
M.D. Mastrandrea, K.J. Mach, G.-K. Plattner, S.K. Allen, M. Tignor, and P.M.
Midgley (eds.)]. Cambridge University Press, Cambridge, UK and New York, NY,
USA, pp. 231-290.
Hanigan, I.C., C.D. Butler, P.N. Kokic, and M.F. Hutchinson, 2012: Suicide and drought
in New South Wales, Australia, 1970-2007. Proceedings of the National
Academy of Sciences of the United States of America, 109(35), 13950-13955.
Hanna, E.G., T. Kjellstrom, C. Bennett, and K. Dear, 2011: Climate change and rising
heat: population health implications for working people in Australia. Asia-
Pacific Journal of Public Health, 23(2 Suppl.), 14S-26S.
Hansen, A.L., P. Bi, P. Ryan, M. Nitschke, D. Pisaniello, and G. Tucker, 2008: The effect
of heat waves on hospital admissions for renal disease in a temperate city of
Australia. International Journal of Epidemiology, 37(6), 1359-1365.
Hashizume, M., 2008: Factors determining vulnerability to diarrhoea during and
after severe floods in Bangladesh. Journal of Water and Health, 6(3), 323-332,
doi:10.2166/wh.2008.062.
Hashizume, M. and A.M. Dewan, 2012: Hydroclimatological variability and dengue
transmission in Dhaka, Bangladesh: a time-series study. BMC Infectious
Diseases, 12(1), 98, doi:10.1186/1471-2334-12-98.
Health Protection Agency, 2012: Health Effects of Climate Change in the UK 2012:
Current Evidence, Recommendations and Research Gaps [Vardoulakis, S. and
C. Heaviside (eds.)]. Health Protection Agency, Public Health England, UK
Government Department of Health, London, UK, 236 pp.

747
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
Heguy, L., M. Garneau, M.S. Goldberg, M. Raphoz, F. Guay, and M. Valois, 2008:
Associations between grass and weed pollen and emergency department visits
for asthma among children in Montreal. Environmental Research, 106(2), 203-
211.
Herrera-Martinez, A.D. and A.J. Rodriguez-Morales, 2010: Potential influence of
climate variability on dengue incidence registered in a western pediatric
hospital of Venezuela. Tropical Biomedicine, 27(2), 280-286.
Hess, J.J., 2008: Climate change: the importance of place. American Journal of
Preventive Medicine, 35(5), 468-478.
Hesterberg, T.W., W.B. Bunn, R.O. McClellan, A.K. Hamade, C.M. Long, and P.A.
Valberg, 2009: Critical review of the human data on short-term nitrogen dioxide
(NO
2
) exposures: evidence for NO
2
no-effect levels. Critical Reviews in Toxicology,
39(9), 743-781.
Hii, Y.L., J. Rocklov, N. Ng, C.S. Tang, F.Y. Pang, and R. Sauerborn, 2009: Climate
variability and increase in intensity and magnitude of dengue incidence in
Singapore. Global Health Action, 2, doi:10.3402/gha.v2i0.2036.
Hii, Y.L., J. Rocklov, and N. Ng, 2011: Short term effects of weather on hand, foot and
mouth disease. PLoS One, 6(2), e16796, doi:10.1371/journal.pone.0016796.
Hii, Y.L., H. Zhu, N. Ng, L.C. Ng, and J. Rocklov, 2012: Forecast of dengue incidence
using temperature and rainfall. PLoS Neglected Tropical Diseases, 6(11), e1908,
doi:10.1371/journal.pntd.0001908.
Holmes, J., 2010: The forestry industry. In: What Do We Know? What Do We Need to
Know? The State of Canadian Research on Work, Employment and Climate
Change [Lipsig-Mummé, C. (ed.)]. Work in a Warming World Research
Programme, Institute for Research and Innovation in Sustainability (IRIS), York
University, Toronto, ON, Canada, pp. 148-166.
Holt, A.C., D.J. Salkeld, C.L. Fritz, J.R. Tucker, and P. Gong, 2009: Spatial analysis of
plague in California: niche modeling predictions of the current distribution and
potential response to climate change. International Journal of Health
Geographics, 8, 38, doi:10.1186/1476-072X-8-38.
Honda, Y., M. Kondo, G. McGregor, H. Kim, Y. Guo, Y. Hijioka, M. Yoshikawa, K. Oka,
S. Takano, S. Hales, and R.S. Kovats, 2013: Heat-related mortality risk model for
climate change impact projection. Environmental Health and Preventive
Medicine, doi:10.1007/s12199-013-0354-6.
Hondula, D.M., J. Rocklov, and O.A. Sankoh, 2012: Past, present, and future climate
at select INDEPTH member Health and Demographic Surveillance Systems in
Africa and Asia. Global Health Action, 5, 74-86.
Hooper, L., C.D. Summerbell, R. Thompson, D. Sills, F.G. Roberts, H.J. Moore, and G.
Davey Smith, 2012: Reduced or modified dietary fat for preventing cardiovascular
disease (Review). Cochrane Database of Systematic Reviews, 5, CD002137,
doi:10.1002/14651858.CD002137.pub3.
Hosking, J. and D. Campbell-Lendrum, 2012: How well does climate change and
human health research match the demands of policymakers? A scoping review.
Environmental Health Perspectives, 120(8), 1076-1082.
Hsieh, Y.H. and C.W. Chen, 2009: Turning points, reproduction number, and impact
of climatological events for multi-wave dengue outbreaks. Tropical Medicine
& International Health, 14(6), 628-638.
Huang, C., A.G. Barnett, X. Wang, P. Vaneckova, G. FitzGerald, and S. Tong, 2011:
Projecting future heat-related mortality under climate change scenarios: a
systematic review. Environmental Health Perspectives, 119(12), 1681-1690.
Huang, C., A.G. Barnett, X. Wang, and S. Tong, 2012: The impact of temperature on
years of life lost in Brisbane, Australia. Nature Climate Change, 2(4), 265-270.
Hughes, B.B., R. Kuhn, C.M. Peterson, D.S. Rothman, J.R. Solorzano, C.D. Mathers,
and J.R. Dickson, 2011: Projections of global health outcomes from 2005 to
2060 using the International Futures integrated forecasting model. Bulletin of
the World Health Organization, 89(7), 478-486.
IFAD, 2010: Rural Poverty Report 2011: New Realities, New Challenges: New
Opportunities for Tomorrow’s Generation. International Fund for Agricultural
Development (IFAD), Rome, Italy, 319 pp.
ILO, 2013: Global Employment Trends 2013: Recovering from a Second Jobs Dip.
International Labour Organization (ILO), Geneva, Switzerland, 170 pp.
IPCC, 2007: Climate Change 2007: The Physical Science Basis. Contribution of
Working Group I to the Fourth Assessment Report of the Intergovernmental
Panel on Climate Change [Solomon, S., D. Qin, M. Manning, Z. Chen, M. Marquis,
K.B. Averyt, M. Tignor, and H.L. Miller (eds.)]. Cambridge University Press,
Cambridge, UK and New York, NY, USA, 996 pp.
IPCC, 2012: Managing the Risks of Extreme Events and Disasters to Advance Climate
Change Adaptation. A Special Report of Working Groups I and II of the
Intergovernmental Panel on Climate Change [Field, C.B., V. Barros, T.F. Stocker,
D. Qin, D.J. Dokken, K.L. Ebi, M.D. Mastrandrea, K.J. Mach, G.-K. Plattner, S.K.
Allen, M. Tignor, and P.M. Midgley (eds.)]. Cambridge University Press,
Cambridge, UK and New York, NY, USA, 582 pp.
Islam, M.S., 2009: Effects of local climate variability on transmission dynamics of
cholera in Matlab, Bangladesh. Transactions of the Royal Society of Tropical
Medicine and Hygiene, 103(11), 1165-1170.
ISO, 1989: Hot Environments – Estimation of the Heat Stress on Working Man, Based
on the WBGT-Index (Wet Bulb Globe Temperature). International Standard ISO
Standard 7243: 1989 E, 2
nd
edn., International Organization for Standardization,
Geneva, Switzerland, 16 pp.
Jackson, J.E., M.G. Yost, C. Karr, C. Fitzpatrick, B.K. Lamb, S.H. Chung, J. Chen, J. Avise,
R.A. Rosenblatt, and R.A. Fenske, 2010: Public health impacts of climate change
in Washington State: projected mortality risks due to heat events and air
pollution. Climate Change, 102(1-2), 159-186.
Jacobson, M.Z., 2009: Review of solutions to global warming, air pollution, and
energy security. Energy & Environmental Science, (2), 148-173.
Jacobson, M.Z., 2010: Short-term effects of controlling fossil-fuel soot, biofuel soot
and gases, and methane on climate, Arctic ice, and air pollution health. Journal
of Geophysical Research: Atmospheres, 115(D14), D14209, doi:10.1029/
2009JD013795.
Jacobson, M.Z., R.W. Howarth, M.A. Delucchi, S.R. Scobie, J.M. Barth, M.J. Dvorak,
M. Klevze, H. Katkhuda, B. Miranda, N.A. Chowdhury, R. Jones, L. Plano, and
A.R. Ingraffea, 2013: Examining the feasibility of converting New York State’s
all-purpose energy infrastructure to one using wind, water, and sunlight. Energy
Policy, 57, 585-601.
Jaenson, T., D. Jaenson, L. Eisen, E. Petersson, and E. Lindgren, 2012: Changes in the
geographical distribution and abundance of the tick Ixodes ricinus during the
past 30 years in Sweden. Parasites & Vectors, 5(1), 8, doi:10.1186/1756-3305-
5-8.
Jakszyn, P., C.A. González, L. Luján-Barroso, M.M. Ros, H.B. Bueno-de-Mesquita, N.
Roswall, A.M. Tjønneland, F.L. Büchner, L. Egevad, K. Overvad, O. Raaschou-
Nielsen, F. Clavel-Chapelon, M. Boutron-Ruault, M.S. Touillaud, J. Chang-Claude,
N.E. Allen, L.A. Kiemeney, T.J. Key, R. Kaaks, H. Boeing, S. Weikert, A.
Trichopoulou, E. Oikonomou, D. Zylis, D. Palli, F. Berrino, P. Vineis, R. Tumino, A.
Mattiello, P.H.M. Peeters, C.L. Parr, I.T. Gram, G. Skeie, M. Sánchez, N. Larrañaga,
E. Ardanaz, C. Navarro, L. Rodríguez, D. Ulmert, R. Ehrnström, G. Hallmans, B.
Ljungberg, A.W. Roddam, S.A. Bingham, K. Khaw, N. Slimani, P.A. Boffetta, M.
Jenab, T. Mouw, D.S. Michaud, and E. Riboli, 2011: Red meat, dietary
nitrosamines, and heme iron and risk of bladder cancer in the European
Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Epidemiology
Biomarkers & Prevention, 20(3), 555-559.
Jakubicka, T., F. Vos, R. Phalkey, M. Marx, and D. Guha-Sapir, 2010: Health Impacts
of Floods in Europe: Data Gaps and Information Needs from a Spatial Perspective.
A MICRODIS Project Report, Universitätsklinikum, Heidelberg, Institut für Public
Health, Heidelberg, Germany and the Center for Research on the Epidemiology
of Disasters (CRED), Université catholique de Louvain (UCL), Brussels, Belgium,
42 pp.
Jamison, D.T., J.G. Breman, A.R. Measham, G. Alleyne, M. Claeson, D.B. Evans, J. Prabhat,
A. Mills, and P. Musgrove (eds.), 2006: Disease Control Priorities in Developing
Countries. 2
nd
edn., The International Bank for Reconstruction and Development
/ The World Bank, Washington, DC, USA and Oxford University Press, New York,
NY, USA, 1401 pp.
Jankowska, M.M., D. Lopez-Carr, C. Funk, and Z.A. Chafe, 2012: Climate change and
human health: spatial modeling availability, malnutrition, and livelihoods in
Mali, Africa. Applied Geography, 33, 4-15.
Jarrett, J., J. Woodcock, U.K. Griffiths, Z. Chalabi, P. Edwards, I. Roberts, and A. Haines,
2012: Effect of increasing active travel in urban England and Wales on costs to
the National Health Service. Lancet, 379(9832), 2198-2205.
Jensen, H., M. Keogh-Brown, R. Smith, Z. Chalabi, A. Dangour, M. Davies, P. Edwards,
T. Garnett, M. Givoni, U. Griffiths, I. Hamilton, J. Jarrett, I. Roberts, P. Wilkinson,
J. Woodcock, and A. Haines, 2013: The importance of health co-benefits in
macroeconomic assessments of UK Greenhouse Gas emission reduction strategies.
Climatic Change, 121(2), 223-237.
Jerrett, M., R.T. Burnett, C.A. Pope 3rd, K. Ito, G. Thurston, D. Krewski, Y. Shi, E. Calle,
and M. Thun, 2009: Long-term ozone exposure and mortality. The New England
Journal of Medicine, 360(11), 1085-1095.
Johnston, F., S. Henderson, Y. Chen, J. Randerson, M. Marlier, R. DeFries, P. Kinney, D.
Bowman, and B. M, 2012: Estimated global mortality attributable to smoke
from landscape fires. Environmental Health Perspectives, 120(5), 695-701.

748
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Jonkman, S.N. and I. Kelman, 2005: An analysis of the causes and circumstances of
flood disaster deaths. Disasters, 29(1), 75-97.
Kaczynski, A.T. and K.A. Henderson, 2008: Parks and recreation settings and active
living: a review of associations with physical activity function and intensity.
Journal of Physical Activity & Health, 5(4), 619-632.
Karanikolos, M., P. Mladovsky, J. Cylus, S. Thomson, S. Basu, D. Stuckler, J.P. Mackenbach,
and M. McKee, 2013: Financial crisis, austerity, and health in Europe. Lancet,
381(9874), 1323-1331.
Kearney, M., W.P. Porter, C. Williams, S. Ritchie, and A.A. Hoffmann, 2009: Integrating
biophysical models and evolutionary theory to predict climatic impacts on
species’ ranges: the dengue mosquito Aedes aegypti in Australia. Functional
Ecology, 23(3), 528-538.
Keim, M.E., 2008: Building human resilience: the role of public health preparedness
and response as an adaptation to climate change. American Journal of Preventive
Medicine, 35(5), 508-516.
Kellenberg, D.K. and A.M. Mobarak, 2008: Does rising income increase or decrease
damage risk from natural disasters? Journal of Urban Economics, 63(3), 788-
802.
Kelly-Hope, L.A., J. Hemingway, and F.E. McKenzie, 2009: Environmental factors
associated with the malaria vectors Anopheles gambiae and Anopheles funestus
in Kenya. Malaria Journal, 8, 268, doi:10.1186/1475-2875-8-2681-8.
Kessler, R.C., S. Galea, M.J. Gruber, N.A. Sampson, R.J. Ursano, and S. Wessely, 2008:
Trends in mental illness and suicidality after Hurricane Katrina. Molecular
Psychiatry, 13(4), 374-384.
Khan, M.S.A., 2008: Disaster preparedness for sustainable development in
Bangladesh. Disaster Prevention and Management, 17(5), 662-671.
Khetsuriani, N., A. LaMonte-Fowlkes, M.S. Oberste, and M.A. Pallansch, 2006:
Enterovirus surveillance – United States, 1970-2005. MMWR Surveillance
Summaries, 55(SS-8), 1-20.
Kim, Y., H. Kim, and D.S. Kim, 2011: Association between daily environmental
temperature and suicide mortality in Korea (2001-2005). Psychiatry Research,
186(2-3), 390-396.
Kinney, P.L., M. Pascal, R. Vautard, and K. Laaidi, 2012: La mortalite hivernale va-t-
elle diminuer avec le changement climatique? [Winter mortality in a changing
climate: will it go down?]. Bulletin épidémiologique hebdomadaire, (12-13),
149-151.
Kinney, P.L., M.S. O’Neill, M.L. Bell, and J. Schwartz, 2008: Approaches for estimating
effects of climate change on heat-related deaths: challenges and opportunities.
Environmental Science & Policy, 11(1), 87-96.
Kite-Powell, H.L., L.E. Fleming, L.C. Backer, E.M. Faustman, P. Hoagland, A. Tsuchiya,
L.R. Younglove, B.A. Wilcox, and R.J. Gast, 2008: Linking the oceans to public
health: current efforts and future directions. Environmental Health, 7(Suppl. 2),
S6, doi:10.1186/1476-069X-7-S2-S6.
Kjellstrom, T. and J. Crowe, 2011: Climate change, workplace heat exposure, and
occupational health and productivity in Central America. International Journal
of Occupational & Environmental Health, 17(3), 270-281.
Kjellstrom, T., I. Holmer, and B. Lemke, 2009a: Workplace heat stress, health and
productivity – an increasing challenge for low and middle-income countries
during climate change. Global Health Action, 2(1), 6, doi:10.3402/gha.v2i0.2047.
Kjellstrom, T., R.S. Kovats, S.J. Lloyd, T. Holt, and R.S. Tol, 2009b: The direct impact of
climate change on regional labor productivity. Archives of Environmental and
Occupational Health, 64(4), 217-227, doi:10.1080/19338240903352776.
Kjellstrom, T., B. Lemke, and O. Hyatt, 2011: Increased workplace heat exposure due
to climate change. Asia-Pacific Newsletter on Occupational Health and Safety,
(18), 6-20.
Kjellstrom, T., B. Lemke, and M. Otto, 2013: Mapping occupational heat exposure
and effects in South-East Asia: ongoing time trends 1980-2009 and future
estimates to 2050. Industrial Health, 51, 56-67.
Knowlton, K., B. Lynn, R.A. Goldberg, C. Rosenzweig, C. Hogrefe, J.K. Rosenthal, and
P.L. Kinney, 2007: Projecting heat-related mortality impacts under a changing
climate in the New York City region. American Journal of Public Health, 97(11),
2028-2034.
Knowlton, K., M. Rotkin-Ellman, G. King, H.G. Margolis, D. Smith, G. Solomon, R. Trent,
and P. English, 2009: The 2006 California heat wave: impacts on hospitalizations
and emergency department visits. Environmental Health Perspectives, 117(1),
61-67.
Knox, J., T. Hess, A. Daccache, and T. Wheeler, 2012: Climate change impacts on crop
productivity in Africa and South Asia. Environmental Research Letters, 7(3),
034032, doi:10.1088/1748-9326/7/3/034032.
Kolstad, E. and K.A. Johansson, 2011: Uncertainties associated with quantifying climate
change impacts on human health: a case study for diarrhea. Environmental
Health Perspectives, 119(3), 299-305.
Kosatsky, T., 2005: The 2003 European heat waves. Eurosurveillance, 10(7), 148-149.
Kovats, R.S. and S. Hajat, 2008: Heat stress and public health: a critical review. Annual
Review of Public Health, 29, 41-55.
Kovats, R.S., S.J. Edwards, S. Hajat, B.G. Armstrong, and K.L. Ebi, 2004: The effect of
temperature on food poisoning: a time-series analysis of salmonellosis in ten
European countries. Epidemiology and Infection, 132, 443-453.
Kozuki, N., A. Lee, M. Silveira, C. Victora, L. Adair, J. Humphrey, R. Ntozini, R. Black, J.
Katz, and Child Health Epidemiology Reference Group Small-for-Gestational-
Age-Preterm Birth, Working Group, 2013: The associations of birth intervals
with small-for-gestational-age, preterm, and neonatal and infant mortality: a
meta-analysis. BMC Public Health, 13(Suppl. 3), S3, doi:10.1186/1471-2458-
13-S3-S3.
Kriz, B., M. Maly, C. Benes, and M. Daniel, 2012: Epidemiology of tick-borne
encephalitis in the Czech Republic 1970-2008. Vector-Borne and Zoonotic
Diseases, 12(11), 994-999.
Lai, L.W., 2011: Influence of environmental conditions on asynchronous outbreaks
of dengue disease and increasing vector population in Kaohsiung, Taiwan.
International Journal of Environmental Health Research, 21, 133-146.
Lake, I.R., 2009: A re-evaluation of the impact of temperature and climate change
on foodborne illness. Epidemiology and Infection, 137(11), 1538-1547.
Lake, I.R., L. Hooper, A. Abdelhamid, G. Bentham, A.B.A. Boxall, A. Draper, S.
Fairweather-Tait, M. Hulme, P.R. Hunter, G. Nichols, and K.W. Waldron, 2012:
Climate change and food security: health impacts in developed countries.
Environmental Health Perspectives, 120(11), 1520-1526.
Lam, N.L., Y. Chen, C. Weyant, C. Venkataraman, P. Sadavarte, M.A. Johnson, K.R.
Smith, B.T. Brem, J. Arineitwe, J.E. Ellis, and T.C. Bond, 2012: Household light
makes global heat: high black carbon emissions from kerosene wick lamps.
Environmental Science & Technology, 46(24), 13531-13538.
Lan, Q., R.S. Chapman, D.M. Schreinemachers, L. Tian, and X. He, 2002: Household
stove improvement and risk of lung cancer in Xuanwei, China. Journal of the
National Cancer Institute, 94(11), 826-835.
Lecocq, F. and Z. Shalizi, 2007: Balancing Expenditures on Mitigation of and
Adaptation to Climate Change: An Exploration of Issues Relevant to Developing
Countries. Policy Research Working Paper 4299, The World Bank Development
Research Group, Sustainable Rural and Urban Development Team, Washington,
DC, USA, 42 pp.
Lefohn, A.S., D. Shadwick, and S.J. Oltmans, 2010: Characterizing changes in surface
ozone levels in metropolitan and rural areas in the United States for 1980-2008
and 1994-2008. Atmospheric Environment, 44(39), 5199-5210.
Lemke, B. and T. Kjellstrom, 2012: Calculating workplace WBGT from meteorological
data: a tool for climate change assessment. Industrial Health, 50(4), 267-278.
Lepeule, J., F. Laden, D. Dockery, and J. Schwartz, 2012: Chronic exposure to fine
particles and mortality: an extended follow-up of the Harvard Six Cities Study
from 1974 to 2009. Environmental Health Perspectives, 120(7), 965-970.
Li, S., H. Tao, and Y. Xu, 2011: Abiotic determinants to the spatial dynamics of dengue
fever in Guangzhou. Asia-Pacific Journal of Public Health, 25(3), 239-247.
Likhvar, V., Y. Honda, and M. Ono, 2011: Relation between temperature and suicide
mortality in Japan in the presence of other confounding factors using time-
series analysis with a semiparametric approach. Environmental Health and
Preventive Medicine, 16(1), 36-43.
Lim, S.S., T. Vos, A.D. Flaxman, G. Danaei, K. Shibuya, H. Adair-Rohani, M.A. AlMazroa,
M. Amann, H.R. Anderson, K.G. Andrews, M. Aryee, C. Atkinson, L.J. Bacchus,
A.N. Bahalim, K. Balakrishnan, J. Balmes, S. Barker-Collo, A. Baxter, M.L. Bell,
J.D. Blore, F. Blyth, C. Bonner, G. Borges, R. Bourne, M. Boussinesq, M. Brauer, P.
Brooks, N.G. Bruce, B. Brunekreef, C. Bryan-Hancock, C. Bucello, R. Buchbinder,
F. Bull, R.T. Burnett, T.E. Byers, B. Calabria, J. Carapetis, E. Carnahan, Z. Chafe, F.
Charlson, H. Chen, J.S. Chen, A.T. Cheng, J.C. Child, A. Cohen, K.E. Colson, B.C.
Cowie, S. Darby, S. Darling, A. Davis, L. Degenhardt, F. Dentener, D. Des Jarlais
C., K. Devries, M. Dherani, E.L. Ding, E.R. Dorsey, T. Driscoll, K. Edmond, S.E. Ali,
R.E. Engell, P.J. Erwin, S. Fahimi, G. Falder, F. Farzadfar, A. Ferrari, M.M. Finucane,
S. Flaxman, F.G.R. Fowkes, G. Freedman, M.K. Freeman, E. Gakidou, S. Ghosh,
E. Giovannucci, G. Gmel, K. Graham, R. Grainger, B. Grant, D. Gunnell, H.R.
Gutierrez, W. Hall, H.W. Hoek, A. Hogan, H.D. Hosgood, D. Hoy, H. Hu, B.J.
Hubbell, S.J. Hutchings, S.E. Ibeanusi, G.L. Jacklyn, R. Jasrasaria, J.B. Jonas, H.
Kan, J.A. Kanis, N. Kassebaum, N. Kawakami, Y. Khang, S. Khatibzadeh, J. Khoo,
C. Kok, F. Laden, R. Lalloo, Q. Lan, T. Lathlean, J.L. Leasher, J. Leigh, Y. Li, J.K. Lin,

749
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
S.E. Lipshultz, S. London, R. Lozano, Y. Lu, J. Mak, R. Malekzadeh, L. Mallinger,
W. Marcenes, L. March, R. Marks, R. Martin, P. McGale, J. McGrath, S. Mehta,
Z.A. Memish, G.A. Mensah, T.R. Merriman, R. Micha, C. Michaud, V. Mishra,
K.M. Hanafiah, A.A. Mokdad, L. Morawska, D. Mozaffarian, T. Murphy, M.
Naghavi, B. Neal, P.K. Nelson, J.M. Nolla, R. Norman, C. Olives, S.B. Omer, J.
Orchard, R. Osborne, B. Ostro, A. Page, K.D. Pandey, C.D.H. Parry, E. Passmore,
J. Patra, N. Pearce, P.M. Pelizzari, M. Petzold, M.R. Phillips, D. Pope, C.A. Pope, J.
Powles, M. Rao, H. Razavi, E.A. Rehfuess, J. Rehm, B. Ritz, F.P. Rivara, T. Roberts,
C. Robinson, J. Rodriguez-Portales, I. Romieu, R. Room, L.C. Rosenfeld, A. Roy,
L. Rushton, J.A. Salomon, U. Sampson, L. Sanchez-Riera, E. Sanman, A. Sapkota,
S. Seedat, P. Shi, K. Shield, R. Shivakoti, G.M. Singh, D.A. Sleet, E. Smith, K.R.
Smith, N.J.C. Stapelberg, K. Steenland, H. Stöckl, L.J. Stovner, K. Straif, L. Straney,
G.D. Thurston, J.H. Tran, R. Van Dingenen, A. van Donkelaar, J.L. Veerman, L.
Vijayakumar, R. Weintraub, M.M. Weissman, R.A. White, H. Whiteford, S.T.
Wiersma, J.D. Wilkinson, H.C. Williams, W. Williams, N. Wilson, A.D. Woolf, P. Yip,
J.M. Zielinski, A.D. Lopez, C.J.L. Murray, and M. Ezzati, 2012: A comparative risk
assessment of burden of disease and injury attributable to 67 risk factors and
risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the
Global Burden of Disease Study 2010. Lancet, 380(9859), 2224-2260.
Lin, R.T. and C.C. Chan, 2009: Effects of heat on workers’ health and productivity in
Taiwan. Global Health Action, 2, doi: 10.3402/gha.v2i0.2024.
Lindgren, E. and R. Gustafson, 2001: Tick-borne encephalitis in Sweden and climate
change. Lancet, 358(9275), 16-18.
Liu, C., N. Hofstra, and E. Franz, 2013a: Impacts of climate change on the microbial
safety of pre-harvest leafy green vegetables as indicated by Escherichia coli
O157 and Salmonella spp. International Journal of Food Microbiology, 163(2-3),
119-128.
Liu, Q., X. Liu, Cirendunzhu, A. Woodward, Pengcuociren, L. Bai, Baimaciwang, S. Sang,
Dazhen, F. Wan, L. Zhou, Y. Guo, H. Wu, G. Li, L. Lu, J. Wang, Dawa, C. Chu, and
Xiraoruodeng, 2013b: Mosquitoes established in Lhasa city, Tibet, China.
Parasites and Vectors, 6, 224, doi:10.1186/1756-3305-6-2241-10.
Liu, X., B. Jiang, W. Gu, and Q. Liu, 2011: Temporal trend and climate factors of
hemorrhagic fever with renal syndrome epidemic in Shenyang City, China. BMC
Infectious Diseases, 11, 331, doi:10.1186/1471-2334-11-331.
Lloyd, S.J., R.S. Kovats, and Z. Chalabi, 2011: Climate change, crop yields, and
malnutrition: development of a model to quantify the impact of climate
scenarios on child malnutrition. Environmental Health Perspectives, 119(12),
1817-1823.
Lobell, D.B., W. Schlenker, and J. Costa-Roberts, 2011a: Climate trends and global
crop production since 1980. Science, 333(6042), 616-620.
Lobell, D.B., M. Bänziger, C. Magorokosho, and B. Vivek, 2011b: Nonlinear heat effects
on African maize as evidenced by historical yield trials. Nature Climate Change,
1(1), 42-45.
Lockwood, A.H., 2012: The Silent Epidemic: Coal and the Hidden Threat to Health.
MIT Press, Cambridge, MA, USA, 248 pp.
Lowe, D., K.L. Ebi, and B. Forsberg, 2011: Heatwave early warning systems and adaptation
advice to reduce human health consequences of heatwaves. International Journal
of Environmental Research and Public Health, 8(12), 4623-4648.
Lozano-Fuentes, S., M.H. Hayden, C. Welsh-Rodriguez, C. Ochoa-Martinez, B. Tapia-
Santos, K.C. Kobylinski, C.K. Uejio, E. Zielinski-Gutierrez, L.D. Monache, A.J.
Monaghan, D.F. Steinhoff, and L. Eisen, 2012: The dengue virus mosquito vector
Aedes aegypti at high elevation in Mexico. The American Journal of Tropical
Medicine and Hygiene, 87(5), 902-909.
Lu, L. and H. Lin, 2009: Time series analysis of dengue fever and weather in
Guangzhou, China. BMC Public Health, 9, 395, doi:10.1186/1471-2458-9-395.
Luber, G. and M. McGeehin, 2008: Climate change and extreme heat events.
American Journal of Preventive Medicine, 35(5), 429-435.
Lucas, R.M., P. Valery, I. van der Mei, T. Dwyer, M.P. Pender, B. Taylor, A.-L. Ponsonby,
and The Ausimmune Investigator Group, 2013: Sun exposure over a lifetime in
Australian adults from latitudinally diverse regions. Photochemistry &
Photobiology, 89(3), 737-744.
Luginbuhl, R., L. Jackson, D. Castillo, and K. Loringer, 2008: Heat-related deaths among
crop workers – United States, 1992 - 2006. JAMA: The Journal of the American
Medical Association, 300(9), 1017-1018, doi:10.1001/jama.300.9.1017.
Lukan, M., E. Bullova, and B. Petko, 2010: Climate warming and tick-borne encephalitis,
Slovakia. Emerging Infectious Diseases, 16(3), 524-526.
Lunde, T.M., M.N. Bayoh, and B. Lindtjorn, 2013: How malaria models relate
temperature to malaria transmission. Parasites & Vectors, 6, 20, doi:10.1186/
1756-3305-6-20.
Lutsey, P.L., M.A. Pereira, A.G. Bertoni, N.R. Kandula, and D.R. Jacobs, 2010: Interactions
between race/ethnicity and anthropometry in risk of incident diabetes.
American Journal of Epidemiology, 172(2), 197-204.
Lutz, W., W. Sanderson, and S. Scherbov, 2008: The coming acceleration of global
population ageing. Nature, 451(7179), 716-719.
Lyons, C.L., M. Coetzee, J.S. Terblanche, and S.L. Chown, 2012: Thermal limits of wild
and laboratory strains of two African malaria vector species, Anopheles
arabiensis and Anopheles funestus. Malaria Journal, 11(1), 226, doi:10.1186/
1475-2875-11-226.
Maas, J., R.A. Verheij, S. de Vries, P. Spreeuwenberg, F.G. Schellevis, and P.P.
Groenewegen, 2009: Morbidity is related to a green living environment. Journal
of Epidemiology & Community Health, 63(12), 967-973.
Macdonald, W.W., 1956: Aedes aegypti in Malaysia. II. Larval and adult biology.
Annals of Tropical Medicine and Parasitology, 50(4), 399-414.
MacMillan, K., A.J. Monaghan, T. Apangu, K.S. Griffith, P.S. Mead, S. Acayo, R. Acidri,
S.M. Moore, J.T. Mpanga, R.E. Enscore, K.L. Gage, and R.J. Eisen, 2012: Climate
predictors of the spatial distribution of human plague cases in the West Nile
Region of Uganda. The American Journal of Tropical Medicine and Hygiene,
86(3), 514-523.
Malik, S.M., H. Awan, and N. Khan, 2012: Mapping vulnerability to climate change
and its repercussions on human health in Pakistan. Globalization and Health,
8, 31, doi:10.1186/1744-8603-8-31.
Mallick, D.L., A. Rahman, M. Alam, A.S.M. Juel, A.N. Ahmad, and S.S. Alam, 2005: Case
Study 3: Bangladesh Floods in Bangladesh: a shift from disaster management
towards disaster preparedness. IDS Bulletin, 36(4), 53-70.
Maloney, S. and C. Forbes, 2011: What effect will a few degrees of climate change
have on human heat balance? Implications for human activity. International
Journal of Biometeorology, 55(2), 147-160.
Mangal, T.D., S. Paterson, and A. Fenton, 2008: Predicting the impact of long-term
temperature changes on the epidemiology and control of schistosomiasis: a
mechanistic model. PLoS One, 3(1), e1438, doi:10.1371/journal.pone.0001438.
Markandya, A., B.G. Armstrong, S. Hales, A. Chiabai, P. Criqui, S. Mima, C. Tonne, and P.
Wilkinson, 2009: Public health benefits of strategies to reduce greenhouse-gas
emissions: low-carbon electricity generation. Lancet, 374(9706), 2006-2015.
Marques, A., M.L. Nunes, S.K. Moore, and M.S. Strom, 2010: Climate change and
seafood safety: human health implications. Food Research International, 43(7),
1766-1779.
Martin, D., B. Belanger, P. Gosselin, J. Brazeau, C. Furgal, and S. Dery, 2007: Drinking
water and potential threats to human health in Nunavik: adaptation strategies
under climate change conditions. Arctic, 60(2), 195-202.
McCormack, G. and A. Shiell, 2011: In search of causality: a systematic review of
the relationship between the built environment and physical activity among
adults. International Journal of Behavioral Nutrition and Physical Activity, 8(1),
125, doi:10.1186/1479-5868-8-125.
McCracken, J.P., K.R. Smith, A. Diaz, M.A. Mittleman, and J. Schwartz, 2007: Chimney
stove intervention to reduce long-term wood smoke exposure lowers blood
pressure among Guatemalan women. Environmental Health Perspectives,
115(7), 996-1001.
McDonald, R.I., P. Green, D. Balk, B.M. Fekete, C. Revenga, M. Todd, and M.
Montgomery, 2011: Urban growth, climate change and freshwater availability.
Proceedings of the National Academy of Sciences of the United States of
America, 108(15), 6312-6317.
McMichael, A.J., 2013a: Human health. In: Four Degrees of Global Warming: Australia
in a Hot World [Christoff, P. (ed.)]. Routledge, Abingdon, UK and New York, NY,
USA, 268 pp.
McMichael, A.J., 2013b: Globalization, climate change, and human health. New
England Journal of Medicine, 368(14), 1335-1343.
McMichael, A.J., J.W. Powles, C.D. Butler, and R. Uauy, 2007: Food, livestock production,
energy, climate change, and health. Lancet, 370(9594), 1253-1263.
McMichael, A.J., P. Wilkinson, R.S. Kovats, S. Pattenden, S. Hajat, B. Armstrong, N.
Vajanapoom, E.M. Niciu, H. Mahomed, C. Kingkeow, M. Kosnik, M.S. O’Neill, I.
Romieu, M. Ramirez-Aguilar, M.L. Barreto, N. Gouveia, and B. Nikiforov, 2008:
International study of temperature, heat and urban mortality: the ISOTHURM
project. International Journal of Epidemiology, 37(5), 1121-1131.
McMichael, C., J. Barnett, and A.J. McMichael, 2012: An ill wind? Climate change,
migration, and health. Environmental Health Perspectives, 120(5), 646-654.
Medlock, J.M. and A. Vaux, 2011: Assessing the possible implications of wetland
expansion and management on mosquitoes in Britain. European Mosquito
Bulletin, 29, 38-65.

750
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Meister, K., C. Johansson, and B. Forsberg, 2012: Estimated short-term effects of
coarse particles on daily mortality in Stockholm, Sweden. Environmental Health
Perspectives, 120(3), 431-436.
Michon, P., J.L. Cole-Tobian, and E. Dabod, S. Schoepflin, J. Igu, M. Susapu, N.
Tarongka, P.A. Zimmerman, J.C. Reeder, J.G. Beeson, L. Schofield, C.L. King, and
I. Mueller, 2007: The risk of malarial infections and disease in Papua New
Guinean children. The American Journal of Tropical Medicine and Hygiene,
76(6), 997-1008.
Milojevic, A., B. Armstrong, S. Kovats, B. Butler, E. Hayes, G. Leonardi, V. Murray, and
P. Wilkinson, 2011: Long-term effects of flooding on mortality in England and
Wales, 1994-2005: controlled interrupted time-series analysis. Environmental
Health, 10, 11, doi:10.1186/1476-069X-10-11.
Milojevic, A., B. Armstrong, M. Hashizume, K. McAllister, A. Faruque, M. Yunus, P. Kim
Streatfield, K. Moji, and P. Wilkinson, 2012: Health effects of flooding in rural
Bangladesh. Epidemiology, 23(1), 107-115.
Mitchell, R. and F. Popham, 2007: Greenspace, urbanity and health: relationships in
England. Journal of Epidemiology & Community Health, 61(8), 681-683.
Moore, S.K., N.J. Mantua, and E.P. Salathé Jr., 2011: Past trends and future scenarios
for environmental conditions favoring the accumulation of paralytic shellfish
toxins in Puget Sound shellfish. Harmful Algae, 10(5), 521-529.
Morabito, M., F. Profili, A. Crisci, P. Francesconi, G. Gensini, and S. Orlandini, 2012:
Heat-related mortality in the Florentine area (Italy) before and after the
exceptional 2003 heat wave in Europe: an improved public health response?
International Journal of Biometeorology, 56(5), 801-810.
Morello-Frosch, R., M. Zuk, M. Jerrett, B. Shamasunder, and A.D. Kyle, 2011:
Understanding the cumulative impacts of inequalities in environmental health:
implications for policy. Health Affairs, 30(5), 879-887.
Murray, C.J.L., L.C. Rosenfeld, S.S. Lim, K.G. Andrews, K.J. Foreman, D. Haring, N. Fullman,
M. Naghavi, R. Lozano, and A.D. Lopez, 2012: Global malaria mortality between
1980 and 2010: a systematic analysis. Lancet, 379(9814), 413-431.
Nakazawa, Y., R. Williams, A.T. Peterson, P. Mead, E. Staples, and K.L. Gage, 2007:
Climate change effects on plague and tularemia in the United States. Vector-
Borne and Zoonotic Diseases, 7(4), 529-540.
Neelormi, S., N. Adri, and A. Ahmed, 2009: Gender dimensions of differential health
effects of climate change induced water-logging: a case study from coastal
Bangladesh. Proceedings of IOP Conference Series: Earth and Environmental
Science, 6, 142026, doi:10.1088/1755-1307/6/14/142026.
Nelson, G.C., M.W. Rosegrant, A. Palazzo, I. Gray, C. Ingersoll, R. Robertson, S. Tokgov,
T. Zhu, T.B. Sulser, C. Ringler, S. Msangi, and L. You, 2010: Food Security, Farming
and Climate Change to 2050. Scenarios, Results, Policy Options. International
Food Policy Research Institute (IFPRI), Washington, DC, USA, 131 pp.
Nelson, G.C., M.W. Rosegrant, J. Koo, R. Robertson, T. Sulser, T. Zhu, C. Ringler, S.
Msangi, A. Palazzo, M. Batka, M. Magalhaes, R. Valmonte-Santos, M. Ewing,
and D. Lee, 2009: Climate Change: Impact on Agriculture and Costs of
Adaptation. International Food Policy Research Institute (IFPRI), Washington,
DC, USA, 19 pp.
Nemet, G.F., T. Holloway, and P. Meier, 2010: Implications of incorporating air-quality
co-benefits into climate change policymaking. Environmental Research Letters,
5(1), 014007, doi:10.1088/1748-9326/5/1/014007.
Neria, Y., 2012: Mental health effects of Hurricane Sandy characteristics, potential
aftermath, and response. JAMA: The Journal of the American Medical Association,
308(24), 2571- 2572, doi:10.1001/jama.2012.110700.
Nitschke, M., G. Tucker, A. Hansen, S. Williams, Y. Zhang, and B. Peng, 2011: Impact
of two recent extreme heat episodes on morbidity and mortality in Adelaide,
South Australia: a case-series analysis. Environmental Health, 10(1), 42-51.
Nunn, P.D., 2009: Responding to the challenges of climate change in the Pacific
Islands: management and technological imperatives. Climate Research, 40,
211-231.
O’Brien, K., M. Pelling, A. Patwardhan, S. Hallegatte, A. Maskrey, T. Oki, U. Oswald-
Spring, T. Wilbanks, and P.Z. Yanda, 2012: Toward a sustainable and resilient
future. In: Managing the Risks of Extreme Events and Disasters to Advance
Climate Change Adaptation. A Special Report of Working Groups I and II of the
Intergovernmental Panel on Climate Change [Field, C.B., V. Barros, T.F. Stocker,
D. Qin, D.J. Dokken, K.L. Ebi, M.D. Mastrandrea, K.J. Mach, G.-K. Plattner, S.K.
Allen, M. Tignor, and P.M. Midgley (eds.)]. Cambridge University Press,
Cambridge, UK, and New York, NY, USA, pp. 437-486.
OECD, 2012: OECD Environmental Outlook to 2050: The Consequences of Inaction.
Organisation for Economic Co-operation and Development (OECD), OECD
Publishing, Paris, France, 349 pp.
Ogden, N.H., A. Maarouf, I.K. Barker, M. Bigras-Poulin, L.R. Lindsay, M.G. Morshed,
C.J. O’callaghan, F. Ramay, D. Waltner-Toews, and D.F. Charron, 2006: Climate
change and the potential for range expansion of the Lyme disease vector Ixodes
scapularis in Canada. International Journal for Parasitology, 36(1), 63-70.
Ogden, N.H., L. St-Onge, I.K. Barker, S. Brazeau, M. Bigras-Poulin, D.F. Charron, C.M.
Francis, A. Heagy, L.R. Lindsay, A. Maarouf, P. Michel, F. Milord, C.J. O’Callaghan,
L. Trudel, and R.A. Thompson, 2008: Risk maps for range expansion of the Lyme
disease vector, Ixodes scapularis, in Canada now and with climate change.
International Journal of Health Geographics, 7, 24, doi:10.1186/1476-072X-7-
24.
Ogden, N.H., C. Bounchard, K. Kurtenbach, G. Margos, L.R. Lindsay, L. Trudel, S.
Nguon, and F. Milord, 2010: Active and passive surveillance and phylogenetic
analysis of Borrelia burgdorferi elucidate the process of Lyme disease risk
emergence in Canada. Environmental Health Perspectives, 118(7), 909-914.
Oikonomou, E. and P. Wilkinson, 2012: Modelling the relative importance of the
urban heat island and the thermal quality of dwellings for overheating in
London. Building and Environment, 57, 223-238.
Okuthe, O.S. and G.E. Buyu, 2006: Prevalence and incidence of tick-borne diseases
in smallholder farming systems in the western-Kenya highlands. Veterinary
Parasitology, 141(3-4), 307-312.
Omumbo, J., B. Lyon, S. Waweru, S. Connor, and M. Thomson, 2011: Raised temperatures
over the Kericho tea estates: revisiting the climate in the East African highlands
malaria debate. Malaria Journal, 10(12), doi:10.1186/1475-2875-10-12.
O’Neill, B., B. Liddle, L. Jiang, K.R. Smith, S. Pachauri, M. Dalton, and R. Fuchs, 2012:
Demographic change and CO
2
emissions. Lancet, 380(9837), 157-164.
Ostro, B., S. Rauch, R. Green, B. Malig, and R. Basu, 2010: The effects of temperature
and use of air conditioning on hospitalizations. American Journal of Epidemiology,
172(9), 1053-1061.
Paaijmans, K.P., A.F. Read, and M.B. Thomas, 2009: Understanding the link between
malaria risk and climate. Proceedings of the National Academy of Sciences of
the United States of America, 106(33), 13844-13849.
Paaijmans, K.P., S. Blanford, A.S. Bell, J.I. Blanford, A.F. Read, and M.B. Thomas, 2010:
Influence of climate on malaria transmission depends on daily temperature
variation. Proceedings of the National Academy of Sciences of the United States
of America, 107(34), 15135-15139.
Padmanabha, H., E. Soto, M. Mosquera, C.C. Lord, and L.P. Lounibos, 2010: Ecological
links between water storage behaviors and Aedes aegypti production:
implications for dengue vector control in variable climates. Ecohealth, 7(1),
78-90.
Paerl, H.W., N.S. Hall, and E.S. Calandrino, 2011: Controlling harmful cyanobacterial
blooms in a world experiencing anthropogenic and climatic-induced change.
Science of the Total Environment, 409(10), 1739-1745.
Page, L.A., S. Hajat, and R.S. Kovats, 2007: Relationship between daily suicide counts
and temperature in England and Wales. The British Journal of Psychiatry: The
Journal of Mental Science, 191, 106-112.
Palecki, M.A., S.A. Changnon, and K.E. Kunke, 2001: The nature and impacts of the
July 1999 heat wave in the midwestern United States: learning from the lessons
of 1995. Bulletin of the American Meteorological Society, 82(7), 1353-1367.
Pan, A., Q. Sun, A.M. Bernstein, M.B. Schulze, J.E. Manson, M.J. Stampfer, W.C. Willett,
and F.B. Hu, 2012: Red meat consumption and mortality: results from 2 prospective
cohort studies. Archives of Internal Medicine, 172(7), 555-563.
Pandey, K., 2010: Costs of Adapting to Climate Change for Human Health in
Developing Countries. Discussion Paper No. 11, Economics of Adaptation to
Climate Change (EACC) study, The International Bank for Reconstruction and
Development / The World Bank, Washington, DC, USA, 19 pp.
Paranjothy, S., J. Gallacher, R. Amlot, G.J. Rubin, L. Page, T. Baxter, J. Wight, D. Kirrage,
R. McNaught, and P. SR, 2011: Psychosocial impact of the summer 2007 floods
in England. BMC Public Health, 11(1), 145, doi:10.1186/1471-2458-11-145.
Parsons, K.C., 2003: Human Thermal Environments: The Effects of Hot, Moderate,
and Cold Environments on Human Health, Comfort, and Performance. 2
nd
edn.,
Taylor & Francis, London, UK and New York, NY, USA, 527 pp.
Pascual, M., J.A. Ahumada, L.F. Chaves, X. Rodo, and M. Bouma, 2006: Malaria
resurgence in the East African highlands: temperature trends revisited.
Proceedings of the National Academy of Sciences of the United States of
America, 103(15), 5829-5834.
Patt, A.G., M. Tadross, P. Nussbaumer, K. Asante, M. Metzger, J. Rafael, A. Goujon, and
G. Brundrit, 2010: Estimating least-developed countries’ vulnerability to climate-
related extreme events over the next 50 years. Proceedings of the National
Academy of Sciences of the United States of America, 107(4), 1333-1337.

751
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
Patz, J.A., S.J. Vavrus, C.K. Uejio, and S.L. McLellan, 2008: Climate change and water-
borne disease risk in the Great Lakes region of the U.S. American Journal of
Preventive Medicine, 35(5), 451-458.
Paz, S., 2009: Impact of temperature variability on cholera incidence in Southeastern
Africa, 1971-2006. Ecohealth, 6(3), 340-345.
Pearce, T., J. Ford, F. Duerden, B. Smit, M. Andrachuk, L. Berrang-Ford, and T. Smith,
2011: Advancing adaptation planning for climate change in the Inuvialuit
Settlement Region (ISR): a review and critique. Regional Environmental Change,
11(1), 1-17.
Peduzzi, P., B. Chatenoux, H. Dao, A. De Bono, C. Herold, J. Kossin, F. Mouton, and O.
Nordbeck, 2012: Global trends in tropical cyclone risk. Nature Climate Change,
2(4), 289-294.
Peng, R.D., J.F. Bobb, C. Tebaldi, L. McDaniel, M.L. Bell, and F. Dominici, 2011: Toward
a quantitative estimate of future heat wave mortality under global climate
change. Environmental Health Perspectives, 119(5), 701-706.
Perera, F.P., 2008: Children are likely to suffer most from our fossil fuel addiction.
Environmental Health Perspectives, 116(8), 987-990.
Pettersson, L., J. Boman, P. Juto, M. Evander, and C. Ahlm, 2008: Outbreak of Puumala
virus infection, Sweden. Emerging Infectious Diseases, 14(5), 808-810.
Pham, H.V., H.T. Doan, T.T. Phan, and N.N. Minh, 2011: Ecological factors associated
with dengue fever in a Central Highlands province, Vietnam. BMC Infectious
Diseases, 11, 172, doi:10.1186/1471-2334-11-172.
Piesse, J. and C. Thirtle, 2009: Three bubbles and a panic: an explanatory review of
recent food commodity price events. Food Policy, 34, 119-129.
Pitzer, V.E., C. Viboud, L. Simonsen, C. Steiner, C.A. Panozzo, W.J. Alonso, M.A. Miller,
R.I. Glass, J.W. Glasser, U.D. Parashar, and B.T. Grenfell, 2009: Demographic
variability, vaccination, and the spatiotemporal dynamics of rotavirus
epidemics. Science, 325(5938), 290-294.
Pitzer, V.E., C. Viboud, B.A. Lopman, M.M. Patel, U.D. Parashar, and B.T. Grenfell, 2011:
Influence of birth rates and transmission rates on the global seasonality of
rotavirus incidence. Journal of the Royal Society Interface, 8(64), 1584-1593.
Po, J.Y., J.M. FitzGerald, and C. Carlsten, 2011: Respiratory disease associated with
solid biomass fuel exposure in rural women and children: systematic review
and meta-analysis. Thorax, 66(3), 232-239.
Pokhrel, A.K., M.N. Bates, S.C. Verma, H.S. Joshi, C.T. Sreeramareddy, and K.R. Smith,
2010: Tuberculosis and indoor biomass and kerosene use in Nepal: a case-
control study. Environmental Health Perspectives, 118(4), 558-564.
Polvani, L.M., D.W. Waugh, G.J.P. Correa, and S.W. Son, 2011: Stratospheric ozone
depletion: the main driver of twentieth-century atmospheric circulation changes
in the Southern Hemisphere. Journal of Climate, 24(3), 795-812.
Porter, J.R. and M. Gawith, 1999: Temperatures and the growth and development of
wheat: a review. European Journal of Agronomy, 10(1), 23-36.
Porter, J.R. and M.A. Semenov, 2005: Crop responses to climatic variation.
Philosophical Transactions of the Royal Society B, 360(1463), 2021-2035.
Potts, M. and C.E. Henderson, 2012: Global warming and reproductive health.
International Journal of Gynecology & Obstetrics, 119, 564-567.
Prata, N., 2009: Making family planning accessible in resource-poor settings.
Philosophical Transactions of the Royal Society B, 364(1532), 3093-3099.
PricewaterhouseCoopers, 2012: Too Late for Two Degrees? Low Carbon Economy
Index 2012. PricewaterhouseCoopers (PwC) LLP, London, UK, 13 pp.
Pudpong, N. and S. Hajat, 2011: High temperature effects on out-patient visits and
hospital admissions in Chiang Mai, Thailand. Science of the Total Environment,
409(24), 5260-5267.
Puppim de Oliveira, J.A., 2009: The implementation of climate change related policies
at the subnational level: an analysis of three countries. Habitat International,
33(3), 253-259.
Raffel, T.R., J.M. Romansic, N.T. Halstead, T.A. McMahon, M.D. Venesky, and J.R. Rohr,
2012: Disease and thermal acclimation in a more variable and unpredictable
climate. Nature Climate Change, 3(2), 146-151.
Ramanathan, V. and G. Carmichael, 2008: Global and regional climate changes due
to black carbon. Nature Geoscience, 1(4), 221-227.
Ramin, B.M. and A.J. McMichael, 2009: Climate change and health in sub-Saharan
Africa: a case-based perspective. Ecohealth, 6(1), 52-57.
Ramsey, J.D., 1995: Task performance in heat: a review. Ergonomics, 38(1), 154-165.
Ramsey, J.D. and T.E. Bernard, 2000: Heat stress. In: Patty´s Industrial Hygiene,
Fifth Edition [Harris, R.L. (ed.)]. John Wiley and Sons, New York, NY, USA, pp.
925-985.
Randolph, S.E., 2010: To what extent has climate change contributed to the recent
epidemiology of tick-borne diseases? Veterinary Parasitology, 167(2-4), 92-94.
Ranjit, S. and N. Kissoon, 2011: Dengue hemorrhagic fever and shock syndromes.
Pediatric Critical Care Medicine, 12(1), 90-100.
Reed, J. and B. Ainsworth, 2007: Perceptions of environmental supports on the physical
activity behaviors of university men and women: a preliminary investigation.
The Journal of American College Health, 56(2), 199-204.
Reid, C.E., M.S. O’Neill, C.J. Gronlund, S.J. Brines, D.G. Brown, A.V. Diez-Roux, and J.
Schwartz, 2009: Mapping community determinants of heat vulnerability.
Environmental Health Perspectives, 117(11), 1730-1736.
Ren, C., G.M. Williams, L. Morawska, K. Mengersen, and S. Tong, 2008: Ozone
modifies associations between temperature and cardiovascular mortality:
analysis of the NMMAPS data. Occupational and Environmental Medicine,
65(4), 255-260.
Reyburn, R., D.R. Kim, M. Emch, A. Khatib, L. von Seidlein, and M. Ali, 2011: Climate
variability and the outbreaks of cholera in Zanzibar, East Africa: a time series
analysis. The American Journal of Tropical Medicine and Hygiene, 84(6), 862-
869.
Rinaldo, A., E. Bertuzzo, L. Mari, L. Righetto, M. Blokesch, M. Gatto, R. Casagrandi,
M. Murray, S.M. Vesenbeckh, and I. Rodriguez-Iturbe, 2012: Reassessment of
the 2010-2011 Haiti cholera outbreak and rainfall-driven multiseason projections.
Proceedings of the National Academy of Sciences of the United States of
America, 109(17), 6602-6607.
Rive, N. and K. Aunan, 2010: Quantifying the air quality cobenefits of the clean
development mechanism in China. Environmental Science & Technology,
44(11), 4368-4375.
Rocklov, J. and B. Forsberg, 2009: Comparing approaches for studying the effects of
climate extremes – a case study of hospital admissions in Sweden during an
extremely warm summer. Global Health Action, 2, doi:10.3402/gha.v2i0.20341-
11.
Rocklov, J., B. Forsberg, and K. Meister, 2009: Winter mortality modifies the heat-
mortality association the following summer. The European Respiratory Journal,
33(2), 245-251.
Rocklov, J., K. Ebi, and B. Forsberg, 2011: Mortality related to temperature and
persistent extreme temperatures: a study of cause-specific and age-stratified
mortality. Occupational and Environmental Medicine, 68(7), 531-536.
Rogelj, J., B. Hare, J. Nabel, K. Macey, M. Schaeffer, K. Markmann, and M.
Meinshausen, 2009: Halfway to Copenhagen, no way to 2 °C. Nature Reports
Climate Change, 3(July 2009), 81-83, doi:10.1038/climate.2009.571.
Ronan, K.R., K. Crellin, D.M. Johnston, K. Finnis, D. Paton, and J. Becker, 2008:
Promoting child and family resilience to disasters: effects, interventions and
prevention effectiveness. Children, Youth and Environments, 18(1), 332-
353.
Rundle, A., K.M. Neckerman, L. Freeman, G.S. Lovasi, M. Purciel, J. Quinn, C. Richards,
N. Sircar, and C. Weiss, 2009: Neighborhood food environment and walkability
predict obesity in New York City. Environmental Health Perspectives, 117(3),
442-447.
Russell, R.C., B.J. Currie, M.D. Lindsay, J.S. Mackenzie, S.A. Ritchie, and P.I. Whelan,
2009: Dengue and climate change in Australia: predictions for the future should
incorporate knowledge from the past. Medical Journal of Australia, 190(5),
265-268.
Rutstein, S.O., 2005: Effects of preceding birth intervals on neonatal, infant and
under-five years mortality and nutritional status in developing countries:
evidence from the demographic and health surveys. International Journal of
Gynecology & Obstetrics, 89(Suppl. 1), S7-S24.
Sahu, S., M. Sett, and T. Kjellstrom, 2013: Heat exposure, cardiovascular stress and
work productivity in rice harvesters in India: implications for a climate change
future. Industrial Health, 51(4), 424-431.
Salomon, J.A., H. Wang, M.K. Freeman, T. Vos, A.D. Flaxman, A.D. Lopez, and C.J.
Murray, 2012: Healthy life expectancy for 187 countries, 1990-2010: a
systematic analysis for the Global Burden Disease Study 2010. Lancet,
380(9859), 2144-2162.
Samson, J., D. Berteaux, B.J. McGill, and M.M. Humphries, 2011: Geographic disparities
and moral hazards in the predicted impacts of climate change on human
populations. Global Ecology and Biogeography, 20(4), 532-544.
Sankoh, O. and P. Byass, 2012: The INDEPTH Network: filling vital gaps in global
epidemiology. International Journal of Epidemiology, 41(3), 579-588.
Satish, U., M.J. Mendell, K. Shekhar, T. Hotchi, D. Sullivan, S. Streufert, and W.J. Fisk,
2012: Is CO
2
an indoor pollutant? Direct effects of low-to-moderate CO
2
concentrations on human decision-making performance. Environmental Health
Perspectives, 120(12), 1671-1677.

752
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Sauerborn, R. and K. Ebi, 2012: Climate change and natural disasters – integrating
science and practice to protect health. Global Health Action, 5, 19295, doi:
10.3402/gha.v5i0.19295.
Schlenker, W. and M.J. Roberts, 2009: Nonlinear temperature effects indicate severe
damages to U.S. crop yields under climate change. Proceedings of the National
Academy of Sciences of the United States of America, 106(37), 15594-15598.
Schmier, J.K. and K.L. Ebi, 2009: The impact of climate change and aeroallergens on
children’s health. Allergy and Asthma Proceedings, 30(3), 229-237.
Schnitzler, J., J. Benzler, D. Altmann, I. Muecke, and G. Krause, 2007: Survey on the
population’s needs and the public health response during floods in Germany
2002. Journal of Public Health Management and Practice, 13(5), 461-464.
Schulte, P.A. and H. Chun, 2009: Climate change and occupational safety and health:
establishing a preliminary framework. Journal of Occupational & Environmental
Hygiene, 6(9), 542-554.
Selin, N.E., S. Wu, K.M. Nam, J.M. Reilly, S. Paltsev, R.G. Prinn, and M.D. Webster, 2009:
Global health and economic impacts of future ozone pollution. Environmental
Research Letters, 4, 044014, doi:10.1088/1748-9326/4/4/044014.
Sheffield, P.E., K. Knowlton, J.L. Carr, and P.L. Kinney, 2011: Modeling of regional
climate change effects on ground-level ozone and childhood asthma. American
Journal of Preventive Medicine, 41(3), 251-257 and quiz A3, doi: 10.1016/j.
amepre.2011.04.017.
Sherry, R.A., X. Zhou, S. Gu, J.A. Arnone, D.S. Schimel, P.S. Verburg, L.L. Wallace, and
Y. Luo, 2007: Divergence of reproductive phenology under climate warming.
Proceedings of the National Academy of Sciences of the United States of
America, 104(1), 198-202.
Sherwood, S.C. and M. Huber, 2010: An adaptability limit to climate change due to
heat stress. Proceedings of the National Academy of Sciences of the United
States of America, 107(21), 9552-9555.
Shindell, D., J.C.I. Kuylenstierna, E. Vignati, R. van Dingenen, M. Amann, Z. Klimont,
S.C. Anenberg, N. Muller, G. Janssens-Maenhout, F. Raes, J. Schwartz, G. Faluvegi,
L. Pozzoli, K. Kupiainen, L. Höglund-Isaksson, L. Emberson, D. Streets, V.
Ramanathan, K. Hicks, N.T.K. Oanh, G. Milly, M. Williams, V. Demkine, and D.
Fowler, 2012: Simultaneously mitigating near-term climate change and improving
human health and food security. Science, 335(6065), 183-189.
Shonkoff, S., R. Morello-Frosch, M. Pastor, and J. Sadd, 2011: Environmental health
and equity implications of climate change and mitigation policies in California:
a review of the literature. Climatic Change, 109(Suppl. 1), S485-S503.
Silva, H.R., P.E. Phelan, and J.S. Golden, 2010: Modeling effects of urban heat island
mitigation strategies on heat-related morbidity: a case study for Phoenix,
Arizona, USA. International Journal of Biometeorology, 54(1), 13-22.
Sinha, R., A.J. Cross, B.I. Graubard, M.F. Leitzmann, and A. Schatzkin, 2009: Meat
intake and mortality: a prospective study of over half a million people. Archives
of Internal Medicine, 169(6), 562-571.
Smith, K.R., 2008: Comparative environmental health assessments. Annals of the
New York Academy of Sciences, 1140, 31-39.
Smith, K.R. and K. Balakrishnan, 2009: Mitigating climate, meeting MDGs, and
moderating chronic disease: the health co-benefits landscape. In:
Commonwealth Health Ministers’ Update 2009 [Commonwealth Secretariat
(ed.)]. Commonwealth Secretariat, London, UK, pp. 59-65.
Smith, K.R. and E. Haigler, 2008: Co-benefits of climate mitigation and health
protection in energy systems: scoping methods. Annual Review of Public
Health, 29, 11-25.
Smith, K.R., M. Jerrett, H.R. Anderson, R.T. Burnett, V. Stone, R. Derwent, R.W. Atkinson,
A. Cohen, S.B. Shonkoff, D. Krewski, C.A. Pope III, M.J. Thun, and G. Thurston,
2009: Public health benefits of strategies to reduce greenhouse-gas emissions:
health implications of short-lived greenhouse pollutants. Lancet, 374(9707),
2091-2103.
Smith, K.R., J.P. McCracken, M.W. Weber, A. Hubbard, A. Jenny, L.M. Thompson, J.
Balmes, A. Diaz, B. Arana, and N. Bruce, 2011: Effect of reduction in household
air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised
controlled trial. The Lancet, 378(9804), 1717-1726.
Smith, K.R., H. Frumkin, K. Balakrishnan, C.D. Butler, Z.A. Chafe, I. Fairlie, P. Kinney,
T. Kjellstrom, D.L. Mauzerall, T.E. McKone, A.J. McMichael, and M. Schneider,
2013: Energy and human health. Annual Review of Public Health, 34, 159-188.
Sokolnicki, L.A., N.A. Strom, S.K. Roberts, S.A. Kingsley-Berg, A. Basu, and N.
Charkoudian, 2009: Skin blood flow and nitric oxide during body heating in
type 2 diabetes mellitus. Journal of Applied Physiology, 106(2), 566-570.
Sousa, C.A., M. Clairouin, G. Seixas, B. Viveiros, M.T. Novo, A.C. Silva, M.T. Escoval,
and A. Economopoulou, 2012: Ongoing outbreak of dengue type 1 in the
Autonomous Region of Madeira, Portugal: preliminary report. Eurosurveillance,
17(49), 20333, www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20333.
Stafoggia, M., F. Forastiere, P. Michelozzi, and C.A. Perucci, 2009: Summer
temperature-related mortality: effect modification by previous winter mortality.
Epidemiology, 20(4), 575-583.
Stanke, C., M. Kerac, C. Prudhomme, J. Medlock, and V. Murray, 2013: Health effects
of drought: a systematic review of the evidence. PLOS Current Disasters, June
5, Edition 1, doi:10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b0041.
State Environmental Institution “Mosecomonitoring”, 2010: Air quality
monitoring in Moscow. WHO Collaborating Centre for Air Quality Management
and Air Pollution Control Newsletter, (46), 9-14.
Stenseth, N.C., N.I. Samia, H. Viljugrein, K.L. Kausrud, M. Begon, S. Davis, H. Leirs,
V.M. Dubyanskiy, J. Esper, V.S. Ageyev, N.L. Klassovskiy, S.B. Pole, and K.S. Chan,
2006: Plague dynamics are driven by climate variation. Proceedings of the
National Academy of Sciences of the United States of America, 103(35), 13110-
13115.
Stern, D.I., P.W. Gething, C.W. Kabaria, W.H. Temperley, A.M. Noor, E.A. Okiro, G.D.
Shanks, R.W. Snow, and S.I. Hay, 2011: Temperature and malaria trends in
highland East Africa. PLoS One, 6(9), e24524, doi:10.1371/journal.pone.
0024524.
Stone, B., J.J. Hess, and H. Frumkin, 2010: Urban form and extreme heat events: are
sprawling cities more vulnerable to climate change than compact cities?
Environmental Health Perspectives, 118(10), 1425-1428.
Strand, L.B., A.G. Barnett, and S. Tong, 2012: Maternal exposure to ambient
temperature and the risks of preterm birth and stillbirth in Brisbane, Australia.
American Journal of Epidemiology, 175(2), 99-107.
Suárez-Varela, M., L. Garcia-Marcos Alvarez, M. Kogan, A. González, A. Gimeno, I.
Ontoso, C. Diaz, A. Pena, B. Aurrecoechea, R. Monge, A. Quiros, J. Garrido, I.
Canflanca, and Á. Varela, 2008: Climate and prevalence of atopic eczema in
6- to 7-year-old school children in Spain. ISAAC PhASE III. International Journal
of Biometeorology, 52(8), 833-840.
Sudre, B., M. Rossi, W. Van Bortel, K. Danis, A. Baka, and N. Vakalis, 2013: Mapping
environmental suitability for malaria transmission, Greece. Emerging Infectious
Diseases, 19(5), 784-786, doi:10.3201/eid1905.120811.
Sumilo, D., A. Bormane, L. Asokliene, V. Vasilenko, I. Golovljova, T. Avsic-Zupanc, Z.
Hubalek, and S.E. Randolph, 2008: Socio-economic factors in the differential
upsurge of tick-borne encephalitis in Central and Eastern Europe. Reviews in
Medical Virology, 18(2), 81-95.
Tagaris, E., K.J. Liao, A.J. Delucia, L. Deck, P. Amar, and A.G. Russell, 2009: Potential
impact of climate change on air pollution-related human health effects.
Environmental Science & Technology, 43(13), 4979-4988.
Tan, J., Y. Zheng, G. Song, L.S. Kalkstein, A.J. Kalkstein, and X. Tang, 2007: Heat wave
impacts on mortality in Shanghai, 1998 and 2003. International Journal of
Biometeorology, 51(3), 193-200.
Tate, J.E., C.A. Panozzo, D.C. Payne, M.M. Patel, M.M. Cortese, A.L. Fowkes, and U.D.
Parashar, 2009: Decline and changes in seasonality of US rotavirus activity after
the introduction of a rotavirus vaccine. Pediatrics, 124(2), 465-471.
Tate, J.E., A.H. Burton, C. Boschi-Pinto, A.D. Steele, J. Duque, U.D. Parashar, and the
WHO-coordinated Global Rotavirus Surveillance Network, 2012: 2008 estimate
of worldwide rotavirus-associated mortality in children younger than 5 years
before the introduction of universal rotavirus vaccination programmes: a
systematic review and meta-analysis. The Lancet Infectious Diseases, 12(2),
136-141.
Teague, B., R. McLeod, and S. Pascoe, 2010: 2009 Victorian Bushfires Royal
Commission Final Report: Summary. Parliament of Victoria, 2009 Victorian
Bushfires Royal Commission, Melbourne, Australia, 42 pp.
Teixeira, E.I., G. Fischer, and H. van Velthuizen, 2011: Global hot-spots of heat stress
on agricultural crops due to climate change. Agricultural and Forest Meteorology,
170, 206-215.
Thompson, A.A., L. Matamale, and S.D. Kharidza, 2012: Impact of climate change
on children’s health in Limpopo Province, South Africa. International Journal
of Environmental Research and Public Health, 9, 831-854.
Thomson, M.C., F.J. Doblas-Reyes, S.J. Mason, R. Hagedorn, S.J. Connor, T. Phindela,
A.P. Morse, and T.N. Palmer, 2006: Malaria early warnings based on seasonal
climate forecasts from multi-model ensembles. Nature, 439(7076), 576-579.
Thornton, P., P. Jones, T. Owiyo, R. Kruska, M. Herrero, O. V, S. Bhadwal, P. Kristjanson,
A. Notenbaert, and N. Bekele, 2008: Climate change and poverty in Africa:
mapping hotspots of vulnerability. African Journal of Agriculture and Resource
Economics, 2(1), 24-44.

753
Human Health: Impacts, Adaptation, and Co-Benefits Chapter 11
11
Tilman, D., R. Socolow, J.A. Foley, J. Hill, E. Larson, L. Lynd, S. Pacala, J. Reilly, T.
Searchinger, C. Somerville, and R. Williams, 2009: Beneficial biofuels – the food,
energy, and environment trilemma. Science, 325(5938), 270-271.
Tirado, M.C., R. Clarke, L.A. Jaykus, A. McQuatters-Gollop, and J.M. Frank, 2010:
Climate change and food safety: A review. Climate Change and Food Science,
43(7), 1745-1765.
Tokarevich, N.K., A.A. Tronin, O.V. Blinova, R.V. Buzinov, V.P. Boltenkov, E.D. Yurasova,
and J. Nurse, 2011: The impact of climate change on the expansion of Ixodes
persulcatus habitat and the incidence of tick-borne encephalitis in the north
of European Russia. Global Health Action, 4, 8448, doi:10.3402/gha.v4i0.
8448.
Tollefsen, P., K. Rypdal, A. Torvanger, and N. Rive, 2009: Air pollution policies in
Europe: efficiency gains from integrating climate effects with damage costs to
health and crops. Environmental Science & Policy, 12(7), 870-881.
Tsai, D.H., J.L. Wang, C.H. Wang, and C.C. Chan, 2008: A study of ground-level ozone
pollution, ozone precursors and subtropical meteorological conditions in central
Taiwan. Journal of Environmental Monitoring, 10(1), 109-118.
Tsui, A.O., A.A. Creanga, and S. Ahmed, 2007: The role of delayed childbearing in the
prevention of obstetric fistulas. International Journal of Gynecology &
Obstetrics, 99(Suppl. 1), S98-S107.
Turcios, R.M., A.T. Curns, R.C. Holman, I. Pandya-Smith, A. LaMonte, J.S. Bresee, R.I.
Glass, and the National Respiratory and Enteric Virus Surveillance System
Collaborating Laboratories, 2006: Temporal and geographic trends of rotavirus
activity in the United States, 1997-2004. The Pediatric Infectious Disease
Journal, 25(5), 451-454.
Uejio, C.K., O.V. Wilhelmi, J.S. Golden, D.M. Mills, S.P. Gulino, and J.P. Samenow, 2011:
Intra-urban societal vulnerability to extreme heat: the role of heat exposure
and the built environment, socioeconomics, and neighborhood stability.
Geographies of Care, 17(2), 498-507.
Ujah, I.A., O.A. Aisien, J.T. Mutihir, D.J. Vanderjagt, R.H. Glew, and V.E. Uguru, 2005:
Factors contributing to maternal mortality in north-central Nigeria: a
seventeen-year review. African Journal of Reproductive Health, 9(3), 27-40.
UN-HABITAT, 2011: Cities and Climate Change: Global Report on Human Settlements
2011. United Nations Human Settlements Programme (UN-HABITAT),
Earthscan, London, UK and Washington, DC, USA, 279 pp.
UNDP, 2011: Human Development Report 2011. Sustainability and Equity: A Better
Future for All. United Nations Development Programme (UNDP), New York, NY,
USA, 185 pp.
UNEP, 2011: Integrated Assessment of Black Carbon and Tropospheric Ozone. United
Nations Environment Programme (UNEP) and World Meteorological Organization
(WMO), UNEP, Nairobi, Kenya and WMO, Geneva, Switzerland, 249 pp.
UNISDR, 2011: 2011 Global Assessment Report on Disaster Risk Reduction: Revealing
Risk, Redefining Development. United Nations International Strategy for
Disaster Reduction (UNISDR), United Nations Office for Disaster Risk Reduction,
Geneva, Switzerland, 178 pp.
van den Berg, A.E., J. Maas, R.A. Verheij, and P.P. Groenewegen, 2010: Green space
as a buffer between stressful life events and health. Social Science & Medicine,
70(8), 1203-1210.
van der Leun, J.C., R.D. Piacentini, and F.R. de Gruijl, 2008: Climate change and
human skin cancer. Photochemical & Photobiological Sciences, 7(6), 730-733.
van Dillen, S.M.E., S. de Vries, P.P. Groenewegen, and P. Spreeuwenberg, 2011:
Greenspace in urban neighbourhoods and residents’ health: adding quality to
quantity. Journal of Epidemiology and Community Health, 66(6), e8, doi:10.1136/
jech.2009.104695.
Van Kerkhove, M.D., K.A.H. Vandemaele, V. Shinde, G. Jaramillo-Gutierrez, A.
Koukounari, C.A. Donnelly, L.O. Carlino, R. Owen, B. Paterson, L. Pelletier, J.
Vachon, C. Gonzalez, Y. Hongjie, F. Zijian, K.C. Shuk, A. Au, S. Buda, G. Krause,
W. Haas, and I. Bonmarin, 2011: Risk factors for severe outcomes following
2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Medicine,
8(7), doi:10.1371/journal.pmed.1001053 1-12.
Van Kleef, E., H. Bambrick, and S. Hales, 2010: The geographic distribution of dengue
fever and the potential influence of global climate change. TropIKA.net, 1(1),
journal.tropika.net/scielo.php?script=sci_arttext&pid=S2078-8606201000
5000001&lng=en.
Vedal, S. and S.J. Dutton, 2006: Wildfire air pollution and daily mortality in a large
urban area. Environmental Research, 102(1), 29-35.
Venkataraman, C., A.D. Sagar, G. Habib, N. Lam, and K.R. Smith, 2010: The Indian
national initiative for advanced biomass cookstoves: the benefits of clean
combustion. 14(2), 63-72.
Vezzulli, L., I. Brettar, E. Pezzati, P.C. Reid, R.R. Colwell, M.G. Hofle, and C. Pruzzo,
2012: Long-term effects of ocean warming on the prokaryotic community:
evidence from the vibrios. ISME Journal: Multidisciplinary Journal of Microbial
Ecology, 6(1), 21-30.
Wang, H., L. Dwyer-Lindgren, K.T. Lofgren, J.K. Rajaratnam, J.R. Marcus, A. Levin-
Rector, C.E. Levitz, A. Lopez, and C.J.L. Murray, 2012: Age-specific and sex-
specific mortality in 187 countries, 1970-2010: a systematic analysis for the
Global Burden of Disease Study 2010. Lancet, 380, 2071-2094.
Wang, X., R. Chen, X. Meng, F. Geng, C. Wang, and H. Kan, 2013: Associations
between fine particle, coarse particle, black carbon and hospital visits in a
Chinese city. Science of the Total Environment, 458-460, 1-6, doi:10.1016/
j.scitotenv.2013.04.008.
Weis, K.E., 2011: Vibrio illness in Florida, 1998-2007. Epidemiology and Infection,
139(4), 591-598.
Weisent, J., W. Seaver, A. Odoi, and B. Rohrbach, 2010: Comparison of three time-
series models for predicting campylobacteriosis risk. Epidemiology and
Infection, 138(6), 898-906.
Weisskopf, M.G., H.A. Anderson, S. Foldy, L.P. Hanrahan, K. Blair, and T.J. Török, 2002:
Heat wave morbidity and mortality, Milwaukee, Wis, 1999 vs 1995: an improved
response? American Journal of Public Health, 29(5), 830-833.
West, J.J., A.M. Fiore, V. Naik, L.W. Horowitz, M.D. Schwarzkopf, and D.L. Mauzerall,
2007a: Ozone air quality and radiative forcing consequences of changes in
ozone precursor emissions. Geophysical Research Letters, 34(6), L06806,
doi:10.1029/2006GL029173.
West, J.J., S. Szopa, and D.A. Hauglustaine, 2007b: Human mortality effects of future
concentrations of tropospheric ozone. Comptes Rendus de l’Academe des
Sciences: Geoscience, 339, 775-783, doi: 10.1016/j.crte.2007.08.005.
West, J.J., A. Fiore, and L. Horowitz, 2012: Scenarios of methane emission reductions
to 2030: abatement costs and co-benefits to ozone air quality and human
mortality. Climatic Change, 114(3-4), 441-461.
West, J.J., S.J. Smith, R.A. Silva, V. Naik, Y. Zhang, Z. Adelman, M.M. Fry, S. Anenberg,
L.W. Horowitz, and J. Lamarque, 2013: Co-benefits of mitigating global
greenhouse gas emissions for future air quality and human health. Nature
Climate Change, 3(10), 885-889.
WHO, 2003: WHO Guide to Cost-Effectiveness Analysis [Tan-Torres Edejer, T., R.
Baltussem, T. Adam, R. Hutubessy, A. Acharya, D.B. Evans, and C.J.L. Murray
(eds.)]. World Health Organization (WHO), Geneva, Switzerland, 318 pp.
WHO, 2006: WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen
Dioxide and Sulfur Dioxide: Global Update 2005. World Health Organization
(WHO), Regional Office for Europe, Copenhagen, Denmark, 484 pp.
WHO, 2008: The Global Burden of Disease. 2004 Update. World Health Organization
(WHO), Geneva, Switzerland, 146 pp.
WHO, 2009a: WHO Guide to Identifying the Economic Consequences of Disease and
Injury. Department of Health Systems Financing, Health Systems and Services,
World Health Organization (WHO), Geneva, Switzerland, 132 pp.
WHO, 2009b: Save Lives: Make Hospitals Safe in Emergencies. WHO/HAC/WHD/
2009.1, World Health Organization (WHO), Geneva, Switzerland, 29 pp.
WHO, 2010: World Malaria Report 2010. Global Malaria Programme, World Health
Organization (WHO), Geneva, Switzerland, 204 pp.
WHO, 2011: Gender, Climate Change and Health. Public Health & Environment
Department (PHE), Health Security & Environment Cluster (HSE), World Health
Organization (WHO), Geneva, Switzerland, 36 pp.
WHO, 2012: World Malaria Report 2012. Global Malaria Programme, World Health
Organization (WMO), Geneva, Switzerland, 249 pp.
WHO, 2013: Impact of Dengue. World Health Organization (WHO), Geneva,
Switzerland, www.who.int/csr/disease/dengue/impact/en/.
WHO and WMO, 2012: Atlas of Health and Climate [Castonguay, S. (ed.)]. World
Health Organization (WHO) and World Meteorological Organization (WMO),
Geneva, Switzerland, 64 pp.
WHO Regional Office for Europe, 2009: Improving Public Health Responses to
Extreme Weather/Heat-Waves – EuroHEAT: Technical Summary. World Health
Organization (WHO) Regional Office for Europe, Copenhagen, Denmark,
60 pp.
WHO Regional Office for Europe, 2010: WHO Guidelines for Indoor Air Quality:
Selected Pollutants. World Health Organization (WHO), Regional Office for
Europe, Copenhagen, Denmark, 454 pp.
WHO Regional Office for Europe, 2013: Climate Change and Health: A Tool to
Estimate Health and Adaptation Costs. World Health Organization (WHO)
Regional Office for Europe, Copenhagen, Denmark, 45 pp.

754
Chapter 11 Human Health: Impacts, Adaptation, and Co-Benefits
11
Wilkinson, P., K.R. Smith, S. Beevers, C. Tonne, and T. Oreszczyn, 2007a: Energy, energy
efficiency, and the built environment. Lancet, 370(9593), 1175-1187.
Wilkinson, P., K.R. Smith, M. Joffe, and A. Haines, 2007b: A global perspective on
energy: health effects and injustices. Lancet, 370(9591), 965-978.
Wilkinson, P., K.R. Smith, M. Davies, H. Adair, B.G. Armstrong, M. Barrett, N. Bruce,
A. Haines, I. Hamilton, T. Oreszczyn, I. Ridley, C. Tonne, and Z. Chalabi, 2009:
Public health benefits of strategies to reduce greenhouse-gas emissions:
household energy. The Lancet, 374(9705), 1917-1929.
Willett, K.M. and S. Sherwood, 2012: Exceedance of heat index thresholds for 15
regions under a warming climate using the wet-bulb globe temperature.
International Journal of Climatology, 32(2), 161-177.
Williams, A.P. and C. Funk, 2011: A westward extension of the warm pool leads to
a westward extension of the Walker circulation, drying eastern Africa. Climate
Dynamics, 37(11-12), 2417-2435.
Woodcock, J., P. Edwards, C. Tonne, B.G. Armstrong, O. Ashiru, D. Banister, S. Beevers,
Z. Chalabi, Z. Chowdhury, A. Cohen, O.H. Franco, A. Haines, R. Hickman, G.
Lindsay, I. Mittal, D. Mohan, G. Tiwari, A. Woodward, and I. Roberts, 2009: Public
health benefits of strategies to reduce greenhouse-gas emissions: urban land
transport. Lancet, 374(9705), 1930-1943.
Woodcock, J., M. Givoni, and A.S. Morgan, 2013: Health impact modelling of active
travel visions for England and Wales using an Integrated Transport and Health
Impact Modelling Tool (ITHIM). Plos One, 8(1), e51462, doi:10.1371/journal.
pone.0051462.
Woodward, A., G. Lindsay, and S. Singh, 2011: Adapting to climate change to sustain
health. WIREs Climate Change, 2(2), 271-282.
World Bank, 2010: World Development Report 2010: Development and Climate
Change. The International Bank for Reconstruction and Development / The
World Bank, Washington, DC, USA, 417 pp.
Wu, F., Q. Liu, L. Lu, J. Wang, X. Song, and D. Ren, 2011: Distribution of Aedes albopictus
(Diptera: Culicidae) in northwestern China. Vector-Borne and Zoonotic Diseases,
11(8), 1181-1186.
Wu, P.C., J.G. Lay, H.R. Guo, C.Y. Lin, S.C. Lung, and H.J. Su, 2009: Higher temperature
and urbanization affect the spatial patterns of dengue fever transmission in
subtropical Taiwan. Science of the Total Environment, 407(7), 2224-2233.
Wyndham, C.H., 1969: Adaptation to heat and cold. Environmental Research, 2(5),
442-469.
Xu, L., Q. Liu, L.C. Stige, T. Ben Ari, X. Fang, K.S. Chan, S. Wang, N.C. Stenseth, and Z.
Zhang, 2011: Nonlinear effect of climate on plague during the third pandemic
in China. Proceedings of the National Academy of Sciences of the United States
of America, 108(25), 10214-10219.
Xu, X., E. Yu, X. Gao, N. Song, L. Liu, X. Wei, W. Zhang, and C. Fu, 2012: Red and
processed meat intake and risk of colorectal adenomas: a meta-analysis of
observational studies. International Journal of Cancer, 132(2), 437-448.
Yoshida, S., T. Satake, and D.S. Mackill, 1981: High-Temperature Stress in Rice. IRRI
Research Paper Series No. 67, International Rice Research Institute (IRRI),
Manila, Philippines, 15 pp.
Zanobetti, A., M.S. O’Neill, C.J. Gronlund, and J.D. Schwartz, 2012: Summer temperature
variability and long-term survival among elderly people with chronic disease.
Proceedings of the National Academy of Sciences of the United States of
America, 10(17), 6608-6613.
Zhang, J. and K. Smith, 2007: Household air pollution from coal and biomass fuels
in China: measurements, health impacts, and interventions. Environmental
Health Perspectives, 115(6), 848-855.
Zhang, Y., P. Bi, and J.E. Hiller, 2010: Climate variations and Salmonella infection in
Australian subtropical and tropical regions. Science of the Total Environment,
408(3), 524-530.
Zhou, S.S., F. Huang, J.J. Wang, S.S. Zhang, Y.P. Su, and L.H. Tang, 2010: Geographical,
meteorological and vectorial factors related to malaria re-emergence in Huang-
Huai River of central China. Malaria Journal, 9, 337, doi: 10.1186/1475-2875-
9-337.
Zhou, X., G. Yang, K. Yang, X. Wang, Q. Hong, L. Sun, J.B. Malone, T.K. Kristensen, N.R.
Bergquist, and J. Utzinger, 2008: Potential impact of climate change on
schistosomiasis transmission in China. American Journal of Tropical Medicine
and Hygiene, 78(2), 188-194.
Zhu, B.P., 2005: Effect of interpregnancy interval on birth outcomes: findings from
three recent US studies. International Journal of Gynecology & Obstetrics,
89(Suppl. 1), S25-S33.
